Overview of Platelet Plug and Blood Clot
Let’s look at the basics of the plug as well as blood clots.
Overview of Platelet Plug and Blood Clot
- Platelet Plug
- Definition: A platelet is an indefinite accumulation of platelets near the location of a fracture in the blood vessel acting as a seal to stop the loss of blood.
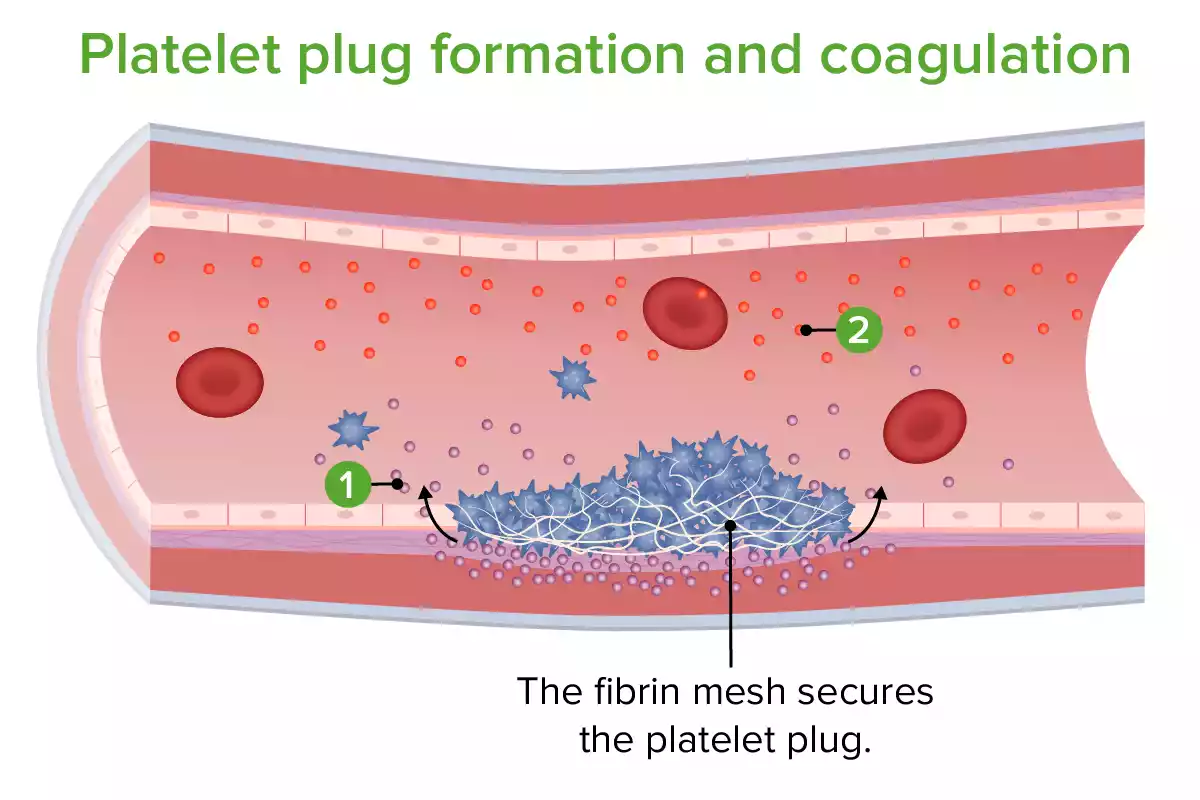
- Formation
- Adhesion: If blood vessels become damaged and exposed, they release the collagen underneath and other substances normally not involved in blood circulation. Platelets stick to the exposed areas.
- activation: Once they are adhered to the site, platelets are activated and release various compounds such as ADP and the thromboxane A2 that draw additional platelets to the website.
- Aggregation: The platelets that are attracted are able to stick together and create the temporary “plug” over the site of injury.
- Role:
- It is the first defense against the loss of blood and allows the body to have time to develop a permanent solution.
- Preparing the site of injury for the eventual formation of blood clots.
- Blood Clot:
- Definition: A blood clot is a mesh made up of mainly fibrin protein, which provides an additional stable seal over the area of injury within the blood vessels. It holds blood cells which include white cells, as well as platelets, effectively halting bleeding.
- Formation:
- A cascade of coagulation: This is a complicated series of enzymatic reactions that involve the clotting factor that leads to the transformation of prothrombin, a soluble protein in plasma, into active form and the thrombin.
- The formation of fibrin: The Thrombin enzyme then facilitates the transformation of fibrinogen soluble, another plasma protein into fibrin strands that are insoluble.
- Cross-linking: The fibrin fibers are linked through factors XIIIA, an enzyme giving strength and stability to the clot.
- Role:
- It creates a stronger seal that will prevent additional loss of blood.
- It’s a long-term solution that ensures the vessel stays sealed, allowing the tissue repair mechanisms to work under the clot barrier that protects it.
- As time passes the clot expands to shrink its size, which aids in wound healing.
The blood clot and platelet plug are designed to stop bleeding, they function in different phases of the hemostatic process and possess distinct roles and compositions. The platelet plug provides a quick, initial response, whereas the blood clot is a more long-lasting, stable solution. Both are crucial to ensure your body’s ability to effectively deal with vascular injuries.
Definition of Hemostasis
Hemostasis can be described as the procedure by which the body ceases bleeding or hemorrhaging. It involves a complicated interplay with the system of vascular platelets (a kind of blood cell that is involved in the process of clotting) as well as various proteins in plasma that together create blood clots.
Hemostasis is divided into three major phases:
- Vascular Phase (Vasoconstriction): Immediately after a blood vessel has been damaged, it expands to limit the flow of blood and reduce the loss of blood. It is a temporary and quick reaction.
- Platelet Phase (Platelet Plug Forming): Platelets adhere to collagen exposed and other elements from the affected vessel. After activation, they release substances that draw more platelets to the area. The platelets accumulate, creating the temporary “platelet plug” over the wound.
- The Coagulation phase (Blood Clot Formation): It involves a series of enzymatic processes that will result in the transformation of fibrinogen from plasma into fibrin threads which pass through the plug of platelets, forming and stabilizing the clot into an even more robust blood clot.
When the injury that caused it is repaired, another process known as fibrinolysis breaks down the clot, making sure that blood flow returns to normal levels.
Hemostasis assures that the body is able to prevent excessive loss of blood due to injuries and also ensures that blood is clear and unhindered when there are no vessel injuries.
What is a Platelet Plug?
A Platelet Plug This is a temporary accumulation of platelets that form on the site of break or injury within the blood vessel. It functions as a first blockage and a “band-aid” to prevent excessive bleeding prior to the more durable and stable form of the blood clot may develop.
Here’s an overview of the plug for platelets
- Formation of the Platelet Plug:
- Adhesion: When blood vessels get damaged, they reveal underlying structures such as collagen and Willebrand factor, which aren’t typically directly contacting blood flow. Platelets stick to the exposed areas, which is the beginning of the formation of a platelet plug.
- activation: After adhesion to the platelets, they are activated. They release several substances, including adenosine dephosphate (ADP) as well as thromboxane A2 and serotonin. These substances are involved in attracting more platelets to areas of injury.
- Aggregation: Newly recruited platelets adhere together, and clump around the site of injury, forming the temporary plug of platelets.
- Role of the Platelet Plug:
- Instant Response: The platelet serves as the body’s initial defense against loss of blood. Before the more robust and durable fibrin clot forms the platelet plug is an immediate response to reduce the loss of blood.
- Coagulation Initiation: Platelets that are activated release substances that trigger the coagulation cascade, which is a sequence of enzymatic processes that lead to the formation of solid fibrin blood clots.
- Limitations and Transition:
- Temporary: The platelet plug is a first and temporary solution. It’s not as sturdy or durable as the fibrin clots that are likely to develop. Imagine the platelet clot as a quick patch-up and allowing the body to develop a permanent solution.
- Setting the stage for Clotting: When the blockage of platelets is present the body is active on its own, releasing the coagulation components needed to create a permanent stable blood clot.
A platelet is the initial stage in the body’s response to vascular injuries, offering an immediate, but short-term solution to the loss of blood and opening the way for the development of a stronger blood clot.
What is a Blood Clot?
A blood clot is a semisolid clot that is formed through the coagulation of blood. It is a complex accumulation of blood constituents, principally composed of platelets, fibrin, and blood cells trapped. Its primary function is to stop the flow of blood (hemostasis) as well, after the injury has healed the body’s mechanisms allow it to dissolve and get rid of the blood clot.
Let’s get deeper into the features and development of blood clots:
- Composition of a Blood Clot:
- Fibrin: Fibrin is an elongated protein that forms an intricate mesh, which is the main structural framework of the clot.
- Platelets: They are tiny blood vessels that perform a crucial role in clotting. In a clot, they are entrapped within the fibrin meshwork and aid in ensuring the stability of the clot.
- blood cells: Red blood cells and, occasionally white blood cells may get stuck in the clot which gives it a maroon or red appearance.
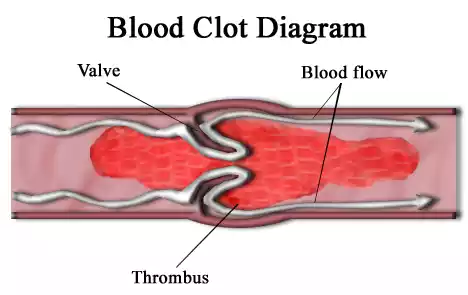
- Formation of a Blood Clot:
- Initiation: The triggers that can trigger the clotting process like a vessel injury that exposes collagen underneath or the release of tissue-related factors from damaged cells.
- The Coagulation Cascade: It is an array of enzymatic reactions with clotting factors. These are proteins typically found in an inactive state inside blood plasma. The cascade eventually leads to an activation process of thrombin which is the key enzyme that is involved in the formation of clots.
- The Fibrin Form: Thrombin is responsible for the transformation of fibrinogen soluble (a plasma-bound protein) into fibrin strands insoluble.
- Clot Stabilization: The fibrin strands crosslink and create an extremely tight mesh. Factor XIIIa is an enzyme that assists in this cross-linking process, further strengthening the clot.
- Role of a Blood Clot:
- Hemostasis: The principal function that a blood clot plays is to stop bleeding and ensure that there is no loss of blood from the sites of injury.
- Tissue Repair: by securing the area of injury, a blood clot creates a favorable environment for tissue repair mechanisms to function under the barrier of clotting.
- Potential Complications and Dissolution:
- Clot Dissolution (Fibrinolysis): Once the wound heals the body begins a process known as fibrinolysis. Plasminogen, which has been incorporated within the clot is activated to produce plasmin. Plasmin will then break down fibrin, causing the dissolution of the clot.
- Thrombosis: Under certain conditions, there is a possibility that clots form in a way that is not appropriate throughout blood vessels causing obstructions. The clots, also known as thrombi, may cause situations such as deep vein thrombosis strokes, pulmonary embolisms, or heart attacks.
The blood clot can be a vital element of the body’s self-repair mechanism that helps prevent excessive loss of blood after traumas. However, the incorrect creation of clots may result in serious health problems.
Platelet Plug and Blood Clot in the comparison chart
Here’s a comparison chart detailing the differences between a platelet plug and a blood clot:
Comparison Chart: Platelet Plug vs. Blood Clot
| Aspect | Platelet Plug | Blood Clot |
|---|---|---|
| Definition | Temporary aggregation of platelets at the site of a vessel injury. | A semisolid mass formed by the coagulation of blood, primarily consisting of fibrin, platelets, and trapped blood cells. |
| Composition | Mainly platelets with some fibrin. | Fibrin meshwork with trapped platelets, red blood cells, and sometimes white blood cells. |
| Formation Mechanism | – Adhesion to exposed vessel structures. – Activation of platelets. – Aggregation of platelets. |
– Initiation by vessel injury or tissue factor release. – Coagulation cascade activation. – Fibrin formation and clot stabilization. |
| Duration & Stability | Temporary and less stable. | Longer-lasting and more stable. |
| Primary Role | Provides a quick, initial response to prevent blood loss at the injury site. | Ensures a durable seal at the injury site, preventing further blood loss and facilitating tissue repair. |
| Appearance | White due to the high concentration of platelets. | Red or maroon because of the trapped red blood cells. |
| Subsequent Stage | Sets the stage for the formation of a blood clot. | Typically contracts and is eventually dissolved by fibrinolysis once healing progresses. |
| Clinical Implications | Short-lived and can be compromised if platelet count or function is impaired (e.g., thrombocytopenia). | Inappropriate clot formation can lead to conditions like deep vein thrombosis, pulmonary embolism, strokes, or heart attacks. |
This chart provides a concise comparison between the platelet plug and the blood clot, emphasizing their definitions, compositions, roles, and other key aspects.
Importance of stopping blood loss after injury
The prevention of blood loss following an injury is essential for a number of reasons that encompass both immediate physiological demands and long-term health benefits.
Here’s an overview of the significance of stopping bleeding:
- Preservation of Blood Volume:
-
- Monitoring Blood Pressure: The blood supply is crucial to ensure that blood pressure is maintained. A substantial loss of blood pressure can result in a decrease in blood pressure (hypotension) and affect the flow of nutrients and oxygen to the vital organs.
- Preventing shock: Blood loss that is excessive could cause hemorrhagic shock which is a serious condition in which the heart is not able to supply sufficient blood to organs.
- Oxygen Delivery:
-
- Red blood cells transport oxygen into tissues. A significant loss of blood can deprive tissues and organs of oxygen, which can cause organ damage or even failure.
- Preventing Infection:
-
- An open wound can be the ideal source of infection for pathogens. Sealing the wound site reduces the chance of infection entering the bloodstream or settling at the wound area.
- Tissue Repair and Healing:
-
- The stopping of blood loss facilitates the beginning of the healing process, which can include inflammation, and then tissue regeneration.
- The blood clot that develops at the site of injury provides the scaffolding for cells that assist in the repair of tissue.
- Maintaining Homeostasis:
-
- Blood plays an essential function in maintaining the internal harmony of our body. This includes the regulation of temperature as well as pH balance and the delivery of nutrients. Loss of blood in excess can disrupt these functions.
- Minimizing Complications:
-
- A high level of blood loss could result in complications like anemia that can lead to fatigue as well as dizziness and pallor. Anemia can also strain the heart, as it attempts to supply enough oxygen to the human body.
- The prevention of excessive blood loss decreases the requirement for blood transfusions which although lifesaving, have certain risks of their own.
- Psychological and Pain Aspects:
-
- A rapid hemostasis procedure can lessen the trauma and pain that can result from injuries. This is crucial in the emergency setting where comfort and stability for the patient are crucial.
- Preventing Further Injury:
-
- In cases that involve internal bleeding stopping the loss of blood is essential to stop the build-up of blood in areas where it shouldn’t go in, for instance, the cerebral cortex (hemorrhagic stroke) or in the abdomen. The accumulation of blood can cause further organ damage or tissue damage.
The prevention of blood loss following injuries is crucial to avoid immediate death as well as long-term health benefits. The body has complex systems such as the platelet plug and coagulation cascade, which ensure quick and efficient hemostasis. If these systems are damaged or if the injuries are serious medical intervention becomes crucial to ensure that adverse effects are not triggered.
Similarities between Platelet Plug and Blood Clot
While the platelet plug as well as blood clots have distinct features and functions for the procedure of hemostatic they share a number of similarities.
Here are some similarities between them:
- Scope: The blood clot and the platelet plug serve to stop blood loss from damaged vessels. They are essential components of the hemostatic reaction to injury.
- Composition: Both rely on platelets as primary elements. When you plug a platelet platelets assemble to form the principal structure. When a blood clot forms, platelets are encased within fiber meshwork.
- Form Site: The plug of platelets and the blood clot are formed on the spot of vascular damage. The platelet plugs first form and is followed by the fibrin-enriched blood clot.
- Initiation: The process is triggered by the exposure of sub-endothelial structures like collagen after the blood vessel is damaged.
- The Coagulation Cascade: The creation of the platelet plug as well as the blood clot are both part that are parts of the cascade for coagulation. Although the formation of the platelet plug relies heavily on platelet activation and aggregation. However, it opens the doorway to the coagulation cascade that ultimately leads to the formation of blood clots.
- Dissolution Mechanism: Both are altered or broken down by the body’s mechanisms for regulation. After healing, the body’s regulatory mechanisms will begin to dissolve or modify the clot, as well as the plug of platelets.
- The Clinical Significance: Both are vital to ensure clinical hemostasis. Conditions that impact the formation of platelet plugs (e.g. the thrombocytopenia syndrome or disorders of platelet function) or the formation of blood clots (e.g. hemophilia) could cause bleeding-related complications.
- Response to medications: The creation of the platelet plug and blood clotting may be affected by antithrombotic drugs. Aspirin, for instance, affects the function of platelets and may affect the formation of platelet plugs, while anticoagulants, such as warfarin, affect the coagulation process in blood clot development.
Although platelet plugs and blood clots play different roles in the hemostatic procedure and are made up of distinct components, they have the primary objective of preventing the loss of blood and are connected in their development and role.
Clinical Implications
The process of platelet plug creation and blood clotting is crucial for hemostasis. But, if these processes are not controlled properly or affected by external influences and conditions, it can lead to important clinical consequences.
Here’s an overview of possible problems in the clinic involving blood clots and platelet plugs:
- Impaired Platelet Plug Formation:
-
- Thrombocytopenia: A decreased number of platelets in the blood can result in insufficient plugs of platelets, which can increase the chance of bleeding.
- Disorders of the Platelet Function: Although there are normal platelet counts, when the platelets aren’t functioning in a way that is optimally (e.g. due to genetic issues medication, or other ailments) the plug for platelets may not be able to form properly.
- Von Willebrand Disease: The deficiency or the dysfunction that affects the von Willebrand factor may cause impairment to the adhesion of platelets to each other, which is an essential stage in the formation of a platelet plug.
- Inappropriate Blood Clotting:
-
- Thrombosis: An abnormal formation of clots within blood vessels may cause conditions such as deep vein thrombosis (DVT) or arterial thrombosis. The clots may block the flow of blood and result in tissue damage.
- Pulmonary Embolism (PE): A clot, most often caused by a DVT, may be transported to the lungs, which can lead to PE, which could be life-threatening.
- Stroke: The formation of blood clots in the arteries that supply the brain may cause strokes that are ischemic.
- Myocardial infarction (Heart attack): Clot formation in coronary arteries could result in a heart attack.
- Impaired Clotting:
-
- Hemophilia: Hemophilia is a genetic disorder that causes blood clotting factors not to function or malfunction, resulting in an extended period of bleeding.
- Vitamin K Deficiency: Vitamin K is crucial for the creation of various factors that clot. Its deficiency can impair blood clotting.
- Liver Disorder: The liver produces the majority of clotting factors. The liver is afflicted by diseases that can hinder its capacity to create these substances, leading to bleeding-related issues.
- Medication-Related Implications:
-
- Anticoagulants: (e.g. warfarin, heparin, or in-oral anticoagulants) These may cause bleeding through hindering the various elements of the coagulation cycle.
- Antiplatelet Drugs: (e.g. aspirin or Clopidogrel) Reduce platelet aggregates and may increase the risk of bleeding.
- Thermolytics: (e.g. tissue plasminogen activator) These medications dissolve clots, and are employed in cases of acute ischemic stroke and myocardial infarction, but they can also increase the chance of bleeding.
- After-surgery and Traumatic bleeding: During surgeries or after traumas that are severe there is a chance of continuing bleeding when the platelet plug and the clotting mechanism don’t work properly.
- Cancer: Certain types of cancer create substances that stimulate the clotting system, which can lead to an increase in the chance of thrombosis. However, certain cancers may also increase the risk of bleeding by infiltrating bone marrow (reducing the production of platelets) or through other mechanisms.
In the clinical setting, knowing the relationship between clot formation and the prevention of excessive bleeding is vital. Both extremes – excessive clotting and insufficient clotting — pose significant risks to health. Proper diagnosis, monitoring, and therapeutic treatments are essential to treat conditions related to blood clots and platelet plugs. clot abnormalities.
Conclusion
The processes involved in the formation of platelet plugs as well as blood clotting are vital for hemostasis and ensure that our bodies are able to respond to injuries to the vascular system. While they are distinct phases in the process of hemostasis they are both interconnected and essential to prevent excessive loss of blood.
The inability to regulate either of these processes can have serious medical implications, from bleeding disorders to potentially life-threatening thrombosis. When it comes to clinical care, maintaining the right balance between clot formation and prevention is essential to ensure patient safety and maximize results.