Clinical considerations in healthcare are important aspects of patient care. These considerations include a wide range of issues, including medical history and diagnosis as well as ethical principles and cultural sensitivity. It is essential to understand and apply these considerations to provide effective and compassionate care.
Importance of understanding the differences between the two drugs
It is important to understand the differences between Bupropion (Bupropion) and Buprenorphine for several reasons:
- Medical Safety: Understanding the differences between drugs allows healthcare professionals to make informed decisions when prescribing medications. This can help prevent harmful drug interactions and the potential harm that could be caused to patients.
- Treatment Efficiency: Different drugs are designed to treat different conditions and have different mechanisms. Understanding the differences can help healthcare providers select the best medication for the patient’s medical condition. This could increase treatment effectiveness.
- Minimizing side effects: Healthcare professionals can choose medications with fewer side effects if they are aware of the different profiles. This can improve treatment compliance and the well-being of patients.
- Legal & Regulatory Considerations: Understanding the legal status of each drug and its regulatory requirements is essential for prescribing a medication. This can lead to legal and ethical implications.
- Addiction Risk: Some medications, such as Buprenorphine may have a greater risk of addiction and dependence than other medications, such as Bupropion. These differences can help healthcare providers make the right decisions for their patients, particularly those who have a history of substance abuse.
- Patient education: Healthcare providers can better educate patients when they understand the differences in medications. Patients who are well informed will be more likely to adhere to their treatment plan and make good decisions regarding their healthcare.
- Optimizing drug therapy: In some cases, patients may take multiple medications simultaneously. Understanding the differences in drugs can help prevent drug-drug interaction and optimize a patient’s medication therapy.
- Accessibility and Cost: Drugs can vary in cost and availability depending on factors like insurance coverage or formulary lists. Understanding these differences can help healthcare providers guide patients to make the most cost-effective decisions.
- Research and Development: Pharmaceutical companies and researchers rely on the understanding of differences between drugs to create new medications and improve those that already exist. For advancements in medical science, it is important to have a deep understanding of the unique properties and how drugs work.
- Making Informed and Ethical Decisions: To practice ethical healthcare, it is important to make informed decisions regarding treatment options. Understanding the differences in drugs is essential to ensure that healthcare professionals are acting in their patients’ interests.
Understanding the differences between drugs will help you provide safe, effective, and ethical healthcare. It allows healthcare professionals to make better decisions, optimize their treatment plans, and improve patient outcomes.
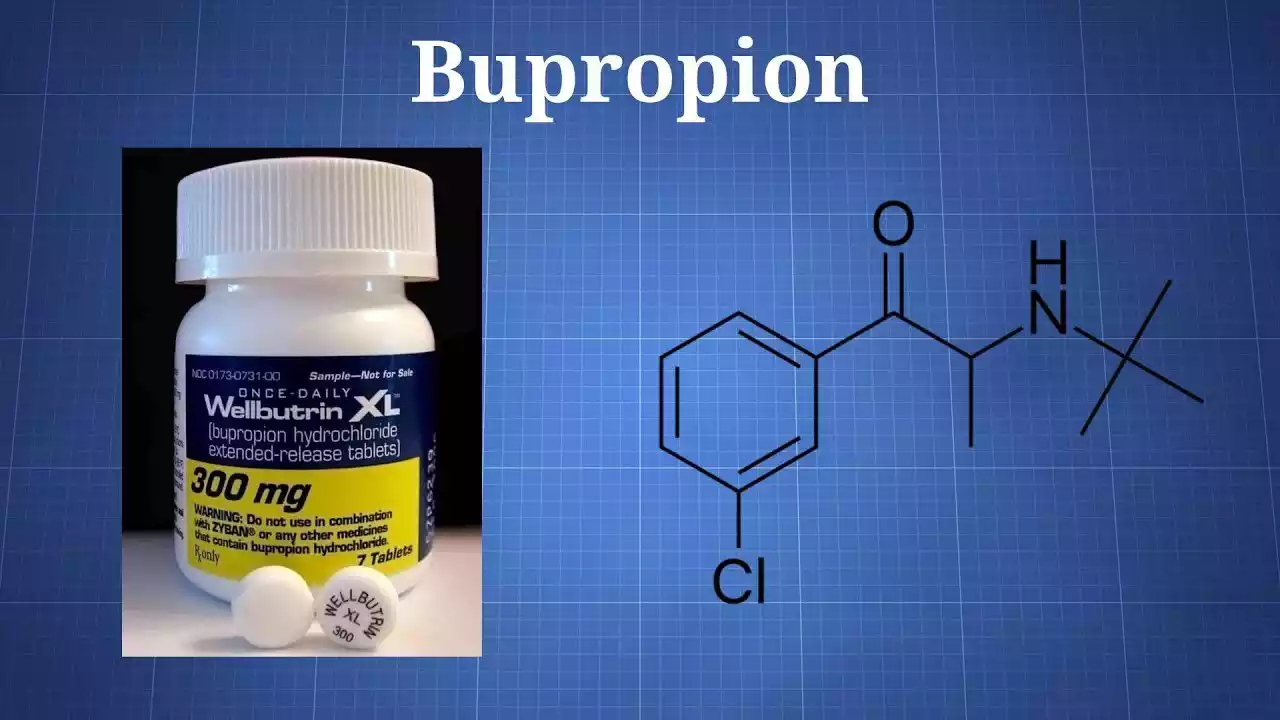
What is Bupropion?
Bupropion can be used to treat depression, and also as a tool for quitting smoking. It is a unique antidepressant with a unique mechanism of action.
Here are some of the key features of Bupropion:
- Generic and Brand Names: The brand name varies depending on the country and formulation. Bupropion is sold under many different brand names, including Wellbutrin Zyban, and Aplenzin.
- Medical Uses:
- Treatment for Depression: Bupropion is a common antidepressant. It affects the balance of neurotransmitters in the brain such as norepinephrine and dopamine, which are responsible for mood regulation.
- Smoking Cessation: Bupropion, sold under the name Zyban is approved as a smoking cessation aid. It reduces withdrawal symptoms and cravings that are associated with nicotine addiction.
- Mechanism: The exact mechanism of action of bupropion is not known, but is thought to involve inhibition of the reuptake of dopamine and norepinephrine. It helps to regulate mood by increasing the availability and effectiveness of these neurotransmitters.
- Indications:
- Bupropion can be used to treat depression when other antidepressants are not effective or cause unwanted side effects.
- It is prescribed for smoking cessation to reduce withdrawal symptoms and cravings.
- Side Effects:
- The side effects of this drug can be varied, but include dry mouth, insomnia, headaches, nausea, dizziness, and increased heart rate.
- Some patients prefer Bupropion because it has fewer side effects sexually compared to other antidepressants.
- Dosage and Administration: The dosage regimen for Bupropion depends on the condition that is being treated and its specific formulation. The medication is usually taken orally and should be prescribed by a healthcare professional.
- Interactions Bupropion may interact with other medications. It is important to tell your doctor about all drugs and supplements that you take to avoid any potential drug interactions.
- Duration: Treatment with Bupropion is dependent on each individual. For depression, the drug is prescribed for several weeks, while smoking cessation is prescribed for a more limited period.
Bupropion must only be taken under the guidance and supervision of a qualified healthcare professional who can monitor your progress and assess your medical needs. Bupropion withdrawal symptoms can occur if you stop abruptly. This is why it’s important to discontinue Bupropion under medical supervision.
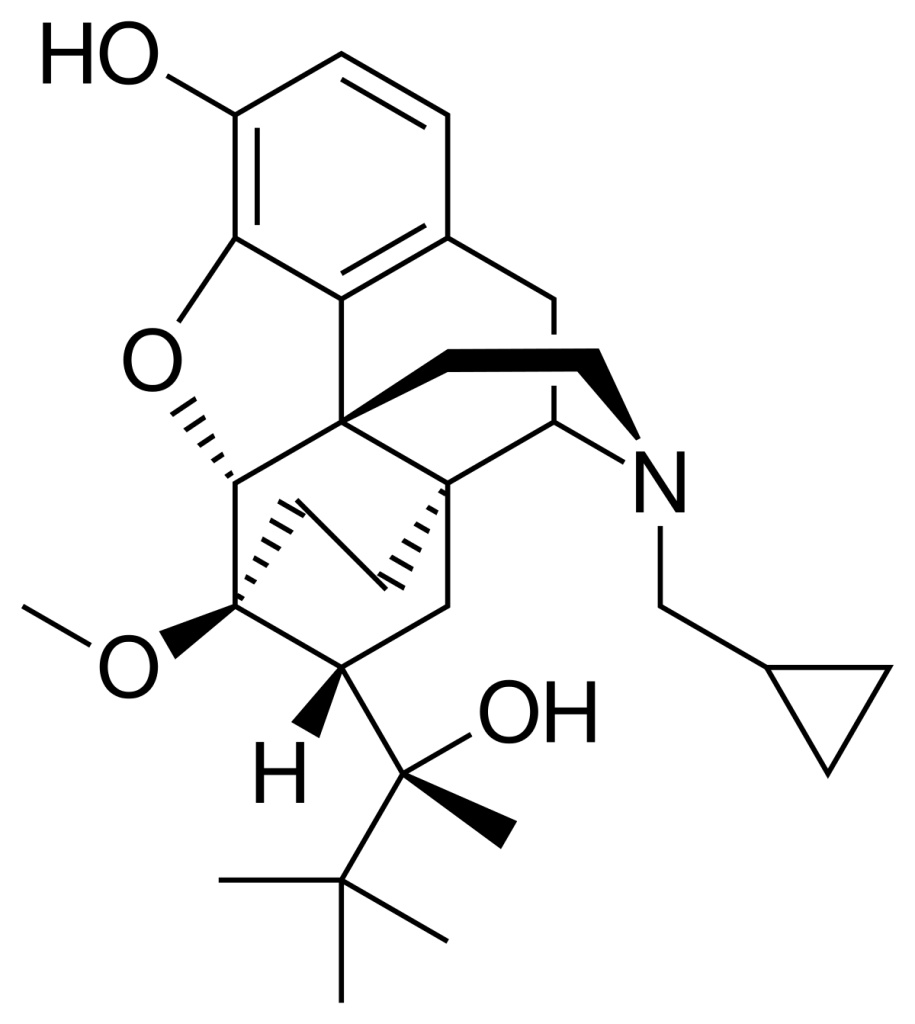
What is Buprenorphine?
Buprenorphine, a medication used to treat opioid addiction, is also prescribed for chronic pain management. This means that it activates the opioid receptors in your brain, but also has a ceiling effect, which limits overdoses and abuse.
Here are some key facts about Buprenorphine:
- Brand and Generic Names: Buprenorphine, the generic name, is also available under the brand names Suboxone Subutex and Belbuca depending on its formulation and intended usage.
- Medical Uses:
- Treatment for Opioid Addiction: Buprenorphine has a primary use in treating opioid use disorder. It reduces opioid cravings and withdrawal syndromes, which makes it easier to stop using illicit opioids.
- Pain management: Buprenorphine can also be used to treat chronic pain in certain formulations, particularly when other medications do not work or have concerns over abuse and addiction.
- Mechanism: Buprenorphine binds to the same opioid receptors in the brain as drugs like heroin or prescription opioids. Its partial agonist properties, however, mean that its effect is limited on these receptors. This reduces the risk of addiction and overdose.
- Indications:
- For Opioid Addiction Treatment: Buprenorphine can be used to treat opioid addiction as part of an overall treatment plan. It can be prescribed by specially trained healthcare professionals in various settings.
- For Pain Management: Buprenorphine-containing formulations may be prescribed by healthcare professionals for chronic pain management when other pain medications are inadequate or inappropriate.
- Side Effects:
- Some side effects include nausea, constipation, and headaches.
- Buprenorphine has a milder respiratory depression than full opioid agonists such as heroin or morphine.
- Dosage and Administration: The dosage regimen for Buprenorphine depends on the formulation and the needs of the patient. The most common form of administration is sublingual films or tablets, although other formulations are available.
- Interactions: Buprenorphine may interact with other medications that affect the liver or central nervous system. To avoid any potential drug interactions, it’s important to tell your doctor about all of the medications and supplements that you take.
- Duration: Buprenorphine treatments for opioid addiction vary greatly from person to person. It can be a short-term treatment to control withdrawal symptoms, or a longer-term maintenance therapy depending on the patient’s goals and needs.
- Regulation: Buprenorphine, a controlled substance is subject to guidelines and regulations aimed at preventing its misuse and diversion.
- Monitoring: Patients receiving Buprenorphine to treat opioid addiction often need regular monitoring from healthcare providers. They must assess the treatment progress and adjust dosages as necessary. They also provide support during recovery.
Buprenorphine can be an important tool for the treatment of opioid addiction. It can help to reduce opioid-related harms and improve the quality of life of those who are addicted. Only a healthcare professional with experience in addiction medicine or chronic pain management should prescribe it.
Bupropion and Buprenorphine in the comparison chart
Here’s a comparison chart highlighting the key differences between Bupropion and Buprenorphine:
| Characteristic | Bupropion | Buprenorphine |
| Generic Name and Brand Names | Bupropion; Wellbutrin, Zyban, Aplenzin, and others | Buprenorphine; Suboxone, Subutex, Belbuca, and others |
| Medical Uses | – Treatment of depression – Smoking cessation aid | – Treatment of opioid use disorder (OUD) – Chronic pain management (in some formulations) |
| Mechanism of Action | – Inhibits reuptake of dopamine and norepinephrine – Affects neurotransmitter balance | – Partial opioid agonist – Activates opioid receptors with a ceiling effect |
| Indications | – Depression that is unresponsive to other antidepressants – Smoking cessation | – Opioid addiction treatment (part of MAT programs) – Chronic pain management (select formulations) |
| Common Side Effects | – Insomnia, dry mouth, headache, nausea, dizziness, increased heart rate | – Nausea, constipation, dizziness, headache, sweating |
| Dosage and Administration | – Orally administered, dosing varies by formulation and condition | – Sublingual tablets, films, and other formulations, dosing varies by formulation and purpose |
| Drug Interactions | – Can interact with other medications and substances | – Can interact with other medications and substances, especially those affecting the central nervous system or liver enzymes |
| Duration of Treatment | – Treatment duration varies, often several months for depression | – Treatment duration varies widely, short-term for withdrawal or long-term for maintenance |
| Legal Status and Regulation | – Regulated, prescription required | – Regulated, prescription required for opioid addiction treatment |
| Addiction and Dependence Risk | – Generally considered low risk for addiction | – Lower risk of addiction compared to full opioid agonists but still carries the potential for misuse |
| Availability and Prescribing | – Prescribed for depression and smoking cessation by healthcare providers | – Prescribed by specially trained healthcare providers for OUD treatment and pain management (with restrictions) |
It’s important to note that these medications serve distinct medical purposes and should only be used under the guidance and prescription of a qualified healthcare provider. Additionally, individual responses to these medications may vary, and the choice between them depends on the specific medical condition and needs of the patient.
Recap of key differences between Bupropion and Buprenorphine
This is a summary of the main differences between Buprenorphine and Bupropion:
Bupropion:
- Primary Usages: The primary use of bupropion is to treat depression and help smokers quit.
- Mechanism: It affects the neurotransmitter equilibrium and inhibits dopamine reuptake in the brain.
- Common side effects: Side effects may include insomnia and dry mouth.
- Indications: Used to treat depression that is not responsive to other antidepressants, and to help quit smoking.
- Addiction risk: is generally considered to be a product with a low addiction risk.
- Dosage: Orally administered, dosage varies depending on the formulation and condition.
- Legal status: Requires a prescription.
- Availability: Prescribed by healthcare providers for depression and smoking quitting.
Buprenorphine:
- Primary Usages: Buprenorphine, or buprenorphine, is used primarily to treat opioid use disorder and in some formulations for chronic pain management.
- Mechanism: This is a partial opioid-agonist that activates opioid receptors, but has a ceiling effect that limits the potential for overdose.
- Common side effects: Side effects may include nausea and constipation.
- Indications: Used to treat OUD as part of medication-assisted treatment (MAT), and in certain formulations for chronic pain management.
- Addiction risk: Although it is less addictive than full opioid agonists it can still be misused.
- Dosage: Administered in the form of sublingual films, tablets, or other formulations. The dosage varies by formulation and use.
- Legal Status: Regulated, and usually requires a prescription for treatment of OUD.
- Availability: Prescribed by specially-trained healthcare providers to treat OUD and manage pain, but with restrictions.
This difference highlights that Buprenorphine and Bupropion are primarily used to treat opioid addiction and in some cases pain management. Buprenorphine also has a partial opioid-agonist mechanism that produces a ceiling effect. This makes it less likely to cause an overdose than full opioid agonists. Both medications are prescribed by doctors and require close monitoring.
Similarities between bupropion and Buprenorphine
Here are a few key similarities between Buprenorphine and Bupropion:
- Prescription Medicines: Both Bupropion (Bupropion) and Buprenorphine (Buprenorphine) are prescription drugs, which means they can only be obtained with a prescription from a doctor.
- Medical Supervision: Both medications must be taken under the supervision and guidance of a qualified healthcare professional. It ensures they are prescribed correctly and that the patients receive appropriate monitoring and support during their treatment.
- Dosage Variability: The dosage for both Bupropion (Buprenorphine) and Buprenorphine may vary depending on the formulation, medical conditions being treated, and the individual patient’s factors. Healthcare providers determine what dosage is appropriate for each patient.
- Drug interactions: Both medications can interact with other substances and drugs. To avoid any potential drug interactions, patients who are using Bupropion or Buprenorphine must inform their healthcare provider about all medications and supplements that they take.
- Regulatory status: Both Bupropion and Buprenorphine, are controlled substances in numerous countries. Both Bupropion and Buprenorphine are regulated as controlled substances in many countries.
- Side Effects: Both Bupropion and Buprenorphine may cause side effects. Individuals can have varying degrees of severity and frequency. The healthcare providers will monitor side effects to adjust the treatment.
- Treatment duration: The length of treatment for both Bupropion and Buprenorphine depends on the medical condition being treated and the individual needs of each patient. The treatment plans are tailored to each patient’s needs to achieve the best possible outcomes.
These similarities, while Bupropion and Buprenorphine have different primary uses and distinct mechanisms of action, highlight the importance of informed and responsible use as well as proper medical supervision and guidance when using these medications.
Clinical Considerations
Healthcare professionals must take clinical considerations into account when they make decisions regarding patient care and treatment. These considerations are based on a mixture of medical evidence and guidelines as well as individual patient characteristics. Here are some clinical considerations that are important in healthcare.
- Patient Assessment and History: The first step is to gather a complete medical history. Understanding the patient’s medical history, current conditions, medications, lifestyle, and psychosocial factors is essential for making informed decisions.
- Differential Diagnosis: This is important for an effective treatment. Differential diagnosis is a process that healthcare providers use to eliminate or confirm specific disorders or diseases.
- Evidence-Based Practice: Clinical decisions should be made based on the best medical evidence available. It is important to stay up-to-date with the latest research, clinical trials, and guidelines.
- Treatment options: It is important to identify and discuss various treatment options with the patient. The provider should take into account the risks, benefits, and expected outcomes for each treatment option, as well as the patient’s values and preferences.
- Informed consent: The ethical and legal requirement to obtain informed consent is the receipt of informed consent. Patients should receive information about proposed treatments, their potential risks, benefits, and alternatives. They should also be able to ask questions and give consent voluntarily.
- Follow-up: It is important to monitor patients regularly during and after their treatment. This includes monitoring the effectiveness of the interventions, evaluating the side effects, and adjusting treatment plans as necessary.
- Individualized care: Healthcare providers recognize that every patient is different and tailor treatment plans according to their needs. They consider factors like age, gender genetics, cultural background, personal preferences, etc.
- Multidisciplinary approach: Complex conditions are often improved by a team-based strategy. Collaboration with nurses, specialists, pharmacists, and other healthcare professionals improves patient outcomes.
- Patient education: It is important to provide patients with information that they can understand about their condition and treatments. Patients who are educated are more likely than others to engage in their care and adhere to treatment plans.
- Ethical considerations: When making decisions regarding treatment and care, healthcare providers should consider ethical principles such as autonomy and beneficence.
- Cultural Competency Understanding and respecting cultural differences is crucial for culturally competent healthcare. Cultural beliefs and practices may influence treatment decisions and compliance with treatment plans.
- Cost & Resource Considerations: Healthcare involves not only clinical decisions but also practical considerations. When making recommendations, providers must take into account the cost of treatment and available resources as well as insurance coverage.
- Legal Compliance: It is important to adhere to the laws and regulations relating to healthcare. It is important to maintain patient privacy (HIPAA for the United States), follow drug scheduling, and meet licensing and accreditation requirements.
The core of high-quality patient-centered care is clinical considerations. They help healthcare professionals make decisions that maximize patient outcomes while taking into account medical, ethical, and practical factors.
Conclusion
The foundation for effective and ethical healthcare is clinical considerations. The holistic approach encompasses a variety of factors, such as accurate diagnosis, evidence-based treatments, individualized plans, ethical principles, and cultural sensitivity. These factors can help healthcare professionals provide the best care to their patients. This ensures both medical effectiveness and patient satisfaction.

