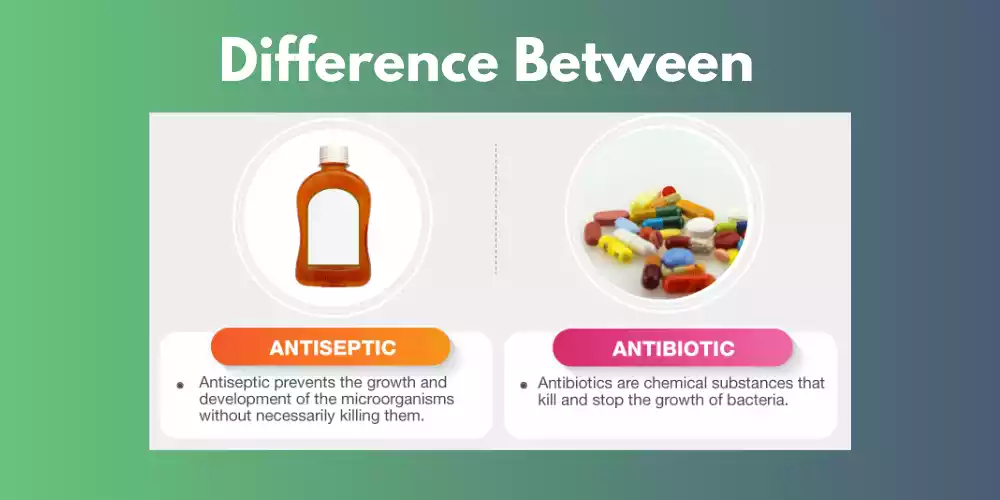
Antibiotics and Antiseptics: The primary difference between antibiotics and disinfectants as well as antiseptics is their mode of action. Antibiotics are absorbed by the body and serve to stop or slow the development and growth of bacteria Antiseptics function externally within the body to block the development and growth of microorganisms however they do not always kill them. In contrast, disinfectants act externally on non-living organisms and eliminate bacteria.
The words antibiotics, antiseptics and disinfectants are all referring to the same phenomenon that inhibits an organism's growth or development, the three types of treatment are used in different ways and the results can differ also.
Definition of Antibiotics

Antibiotics are powerful drugs that play an integral part in fighting bacterial infections in both animals and humans. Their name comes from the Greek antibiosis, meaning "against life", to denote their primary goal inhibiting harmful bacteria growth while saving lives. Antimicrobial substances also exist which can prevent organism development thereby eliminating it entirely.
Antibiotics work by targeting functions or structures essential to bacteria survival, like blocking cell wall production and protein synthesis as well as DNA replication. By interfering with these essential processes, antibiotics actually weaken bacteria, helping the immune system of your body eliminate disease more effectively.
Antibiotics only treat bacterial infections; they do not work against viral ones such as influenza or the common cold. While in the past antibiotics revolutionized medicine by dramatically reducing mortality and morbidity rates associated with bacterial infections, their widespread and often uncontrolled use has led to antibiotic-resistant organisms emerging that pose a grave threat to global health - thus, responsible and correct usage is crucial to ensure continued effectiveness for years to come.
Definition of Antiseptics

Antiseptics, or chemical compounds used to impede the development and activity of microorganisms that inhabit tissues - including mucous membranes and skin. Antiseptics differ from antibiotics in that they're designed specifically to combat bacteria within your body; antiseptics tend to be applied externally, treating infections caused by cuts, wounds or minor injuries on body surfaces such as cuts.
Antiseptics serve the primary purpose of cleaning and disinfecting skin tissues by decreasing or eliminating harmful microorganisms present. This form of medication is often utilized prior to medical procedures as well as daily hygiene practices to decrease the chance of an infection occurring.
Antiseptics work in various ways, such as denaturing proteins, dissolving cell membranes, or interfering with vital metabolic processes of microorganisms such as bacteria, fungi and certain viruses - providing protection from infection.
Antiseptic agents include isopropyl alcohol hydrogen peroxide, povidone-iodine and chlorhexidine - also known as benzalkonium chloride. They come in various forms including wipes, solutions, or creams to ensure easy application and use.
Antiseptics should only be applied externally on healthy skin; internal use or large wounds could result in tissue damage that slows healing. Furthermore, when applying them it is vitally important that proper guidelines and recommendations be observed to maximize effectiveness while minimizing potential negative side effects.
Importance of Differentiating Between the Two
Understanding the difference between antiseptics and antibiotics is vitally important, for many reasons as explained below:
- Understanding the differences between antiseptics and antibiotics can assist health professionals and individuals alike in selecting an appropriate course of treatment for their ailments. Antibiotics work best against bacterial infections while antiseptics help protect skin surfaces against future infection. By choosing the correct therapy plan for a given ailment, healthcare professionals and individuals alike will greatly enhance patient outcomes while decreasing medication requirements.
- Antibiotic Resistance Antibiotic resistance is a serious global health concern. Misusing antibiotics or using them when more effective antiseptics would suffice can contribute to resistant bacteria developing resistance against them; by isolating them from one another you can ensure they only use them when necessary and keep resistance at bay as well as maintaining effectiveness against serious infections.
- Antiseptics play an essential part in infection control in healthcare settings, particularly through proper use on skin and surfaces to stop pathogen transmission and reduce risks of healthcare-associated infections. Healthcare workers can utilize both antiseptics and antibiotics as tools for effective and efficient infection control methods.
- Safety and Side Effect Antibiotics and other antiseptics each have their own safety profiles and adverse side effects, some triggering digestive disturbances or allergic reactions for certain individuals, while incorrect use can irritate mucous membranes or skin. Understanding their difference helps both patients and healthcare professionals use these medications safely while limiting any potential for harm.
- Understanding the difference between antiseptics and antibiotics is of utmost importance when it comes to public health programs. Appropriate use of both can reduce bacteria resistant to antibiotics while saving unnecessary costs related to ineffective treatment plans.
- Clarifying the differences between antiseptics and antibiotics helps increase education and awareness within society at large. When people know when and how best to take these medicines they can better participate in decision-making by their physicians while aiding in efforts against antibiotic resistance.
- With proper treatment comes better outcomes for infections. Antiseptics could help protect from future infection while antibiotics treat any existing ones directly, thus eliminating their source.
Antiseptics and antibiotics must be kept distinct to promote safe use of medications and reduce antibiotic resistance, improve infection control and obtain optimal treatment results. By informing healthcare professionals and the public about these two categories of medication, this process provides better and safer medical practices which benefit patients as well as society as a whole.
Antibiotics
Antibiotics are important tools in modern medicine, serving to treat both human and animal bacterial infections effectively. From common respiratory conditions to life-threatening illnesses, antibiotics play an integral part in keeping society alive.
Antibiotics Feature Key Attributes:
Antibiotics are designed to kill or inhibit the development of bacteria; however, they don't work against viral infections like flu or colds as their structures and lives cycles differ significantly from bacteria's.
- Antibiotics work through multiple mechanisms to interfere with bacterial functions and thus lead to their death. For instance, certain antibiotics inhibit cell wall integrity while others interfere with protein synthesis or DNA replication - all eventually leading to their demise.
- Broad Spectrum and Narrow Spectrum Antibiotics can be divided into two broad-spectrum and narrow-spectrum classes. Broad-spectrum antibiotics attack various kinds of bacteria simultaneously, making them suitable for treating various ailments when their cause remains unknown. Narrow-spectrum antibiotics, on the other hand, target only specific strains of organisms responsible for an infection, making them recommended in cases when an organism's identity has already been determined.
- Available Antibiotics Are Many Varieties There are various classes of antibiotics with their own individual characteristics and mechanism of action; among the more widely-used ones are penicillins, macrolides, tetracyclines, cephalosporins, and fluoroquinolones - each targeting certain bacteria or functions in different ways.
- Antibiotics require a valid prescription from a qualified healthcare provider in order to be used effectively and decrease resistance risk. Proper identification and diagnosis is critical in providing effective and long-lasting treatment solutions, thus decreasing risk.
- Antibiotic Resistance One of the greatest concerns faced by doctors today is antibiotic resistance. Overuse and misuse have contributed to the emergence of resistant bacteria which makes certain diseases harder or even untreatable; for this reason, it is vital that antibiotics only be prescribed when necessary to combat this rising global health threat.
- Like all medications, antibiotics may cause adverse side effects. Common examples are stomach upset and allergies as well as interactions with other drugs. Healthcare providers carefully weigh up the advantages and risks when prescribing them to patients.
- Antibiotics should only be used as a preventative treatment and should be administered in accordance with established guidelines to avoid unnecessary prophylactic use that could increase antibiotic resistance. If antibiotics are being prescribed prophylactically for preoperative procedures or as a prophylactic measure before surgery, however, excessive prophylactic use could increase risks of infection and lead to antibiotic resistance; so excessive use may create this scenario.
Antibiotics have revolutionized medicine and saved many lives with their effective treatment of bacteria-related infections, but misuse and improper usage have caused antibiotic-resistant organisms to emerge that pose an immense threat to public health. Therefore, proper use, diagnosis, and education are crucial components in upholding antibiotic efficacy against further outbreaks of bacterial infections.
Antiseptics
Antiseptics are chemical ingredients designed to clean and disinfect living tissues such as mucous membranes and skin as well as treat infections. Antiseptics are most often applied externally in order to decrease bacteria on surfaces or wounds or limit the spreading of infectious pathogens; in this regard, they differ from disinfectants which typically are only effective against surfaces and objects that have inanimate components.
Key Features of Antiseptics:
Antiseptics provide a broad spectrum of action against bacteria, fungi, and certain viruses.
- Mode of Action Antiseptics works through various mechanisms, such as dissolving proteins, damaging cell membranes, or interfering with microorganisms' vital metabolic processes that ultimately lead to decreased growth rates and the prevention of infections.
- These treatments are applied directly to mucous membranes or skin. There are various types available, including creams, wipes, and sprays; making them easy and simple to use and apply.
- Antiseptics are used in wound care and infection prevention by treating wounds, cleaning out small cuts, abrasions, and burns, and treating small cuts, abrasions or burns that require tending. Furthermore, they may be utilized prior to or during surgical procedures in order to decrease the risk of an infection being transmitted through surgical instruments.
- Antiseptic Agents The most frequently used antiseptics include chlorhexidine, povidone-iodine, and hydrogen peroxide; isopropyl alcohol and benzalkonium chlorine are also often employed, in addition to solutions containing iodine.
- Safety Considerations Antiseptics should generally be safe to use on externally uninjured skin, but should never be applied internally or to large, deep wounds as this could damage tissue and delay the healing process. Some individuals may be sensitive to certain antiseptics; therefore it's essential that all applicable guidelines be observed when applying them.
- Antiseptic ResistanceWhile resistance to antiseptics may not be as prevalent as resistance to antibiotics, prolonged and frequent use can still result in decreased efficacy over time.
Antiseptics play an indispensable role in wound care and infection prevention in many environments - healthcare facilities, households and industries alike. Proper use of antiseptics and following any medical guidelines are crucial to ensure faster healing times while avoiding complications that come with infections.
Comparing Antibiotics and Antiseptics
Comparing antiseptics and antibiotics is critical in understanding their respective functions, mechanisms of action and uses within healthcare. While both products are effective at fighting disease, their goals, uses and efficacies vary considerably - this comparison of antibiotics and antiseptics serves to shed more light on each.
1. Purpose:
- Antibiotics are commonly prescribed to treat infections caused by bacteria within the body, including urinary, respiratory, or bloodstream infections.
- Antiseptics are used to treat or prevent infections on the external surfaces of the body, including cuts, wounds and mucous membranes.
2. Microorganisms Targeted:
- Antibiotics are designed specifically to combat bacteria-borne pathogens.
- Antiseptics can effectively combat an array of microorganisms, including fungi, bacteria and some viruses.
3. Mechanism of Action:
- Antibiotics work by interfering with certain functions performed by bacteria, such as cell wall production, protein synthesis or DNA replication - ultimately leading to either their death or impeding their progress.
- Antiseptics work by breaking down proteins, dismantling cell membranes and disrupting essential metabolic processes that microorganisms perform; ultimately limiting their growth and protecting from infections.
4. Application and Use:
- Antibiotics should be taken orally via tablets or injectables in order to penetrate the bloodstream and fight infection throughout the body.
- For external use on mucous membranes or skin as wipes, solutions, or creams to cleanse and disinfect affected areas.
5. Spectrum of Activity:
- Antibiotics can be divided into broad-spectrum or narrow-spectrum antibiotics depending on their effectiveness against different kinds and strains of bacteria, or against specific ones and types.
- Antiseptics typically possess a broad array of activities and therefore effectively combat microorganisms found on surfaces.
6. Resistance Concerns:
- Misuse and overuse have led to the proliferation of antibiotic-resistant bacteria which pose serious threats to public health.
- Antiseptics Though rare, it is possible to become resistant to antiseptics with prolonged or excessive use.
7. Adverse Reactions and Possible Safety Issues:
- Antibiotics may cause side effects, including gastrointestinal upset or allergic reactions, as well as negative interactions when combined with other medicines.
- While typically intended for external use, some individuals may experience skin irritation or allergies when applying them directly to their skin.
8. Context of Use:
- Antibiotics are prescribed by health professionals based on an accurate diagnosis and the identification of any cause for the bacteria present.
- Antiseptics are widely utilized both at home and in healthcare environments to treat wounds and prevent infections.
Antibiotics and antiseptics both play unique roles in fighting illness. Antibiotics are drugs taken orally for treating bacterial diseases while antiseptics are external substances used to prevent and treat infections on the surface of the body. Understanding their differences is essential for safe use as well as to combat resistance to antibiotics and prevent future outbreaks of infection.
History of Antibiotic and Antiseptic
History of Antibiotics:
Ancient Remedies: Antibiotics can trace their history back thousands of years to when ancient civilizations used plant extracts and molds from nature to treat ailments, while Egyptians and Greeks relied upon items like garlic, honey, and wine-soaked bandages as treatments.
- In 1928, modern antibiotic therapy began when Scottish biochemist Alexander Fleming accidentally discovered penicillin. By finding that Penicillium notatum prevented bacteria growth in a petri dish, Fleming discovered what would later become the world's first effective antibiotic - penicillin!
- During World War II, penicillin's ability to combat bacterial infections was discovered and led to massive efforts at mass-producing the antibiotic. Researchers Florey and Chain were successful in rapidly ramping up production; saving many lives during a time of conflict.
- Discoveries of Other Antibiotics Following the success of penicillin, research for additional antibiotics intensified. In the 1940s and 50s, streptomycin, chloramphenicol, erythromycin, and tetracycline were all discovered, further expanding our arsenal.
- It was widely considered that the 1950s to 1970s was considered to be the era of "golden antibiotics", with numerous new classes emerging during this time and further revolutionizing medicine as a field.
Development of Antibiotic Resistance Over time, antibiotic resistance became an ever-increasing threat as bacteria became resistant to their harmful effects and required increased use of antibiotics and research into new ones for proper usage and production. This necessitated responsible practices when administering them as well as continual research for potential new antibiotics.
History of Antiseptics:
In early civilizations, basic antiseptic measures like boiling water for wound washing and using vinegar or wine as antiseptic wash solutions and applying herbal concoctions against infection were used for antiseptic purposes.
- Ignaz Semmelweis and Handwashing The mid-19th century saw the debut of handwashing practices. Hungarian doctor Ignaz Semmelweis noted a reduction in mortality rates after physicians cleansed their hands with chlorine solutions before treating pregnant women - this became one of the earliest steps towards modern antiseptic methods.
- Joseph Lister and Antiseptic Surgery In the 1860s, British surgeon Joseph Lister pioneered antiseptic surgery by employing carbolic acid (phenol) to clean surgical instruments, cuts, and dressings after each surgical procedure - leading to an impressive decrease in postoperative infections.
- With research progressing, new antiseptic agents such as hydrogen peroxide, chlorhexidine, and iodine were produced as more efficient ways of healing wounds and warding off infections were discovered.
- Antiseptic practices have become a standard part of medical facilities, helping reduce infections during surgical procedures and improving outcomes for patients. Antiseptics are also often employed for daily wound treatments and personal hygiene needs.
- Innovative Formulations of Antiseptics In recent times, antiseptics have been introduced into different products - alcohol-based hand soaps and wipes being two examples - making these more accessible and convenient than ever for the public.
Antibiotics and antiseptics have marked significant milestones in medical history, revolutionizing treatment and improving public health. While antibiotics have saved many lives by curing infections as well as preventing their spread, antiseptics play a vital role in disease prevention by slowing the transmission of disease-causing pathogens across different environments. Continued research into these drugs' efficacy as well as prudent use is vital to maintain its efficacy against emerging challenges like antimicrobial resistance.
Safety and Proper Use of Antibiotic and Antiseptic
The use of antiseptics and antibiotics is essential in order to ensure they are effective, prevent adverse reactions, and decrease the possibility of antibiotic resistance.
Here are guidelines to ensure their safe and responsible usage:
Safety and Appropriate Usage of Antibiotics:
Healthcare Professionals Should Prescribe Antibiotics Antibiotics should only be prescribed by licensed health professionals who can clearly diagnose and identify specific bacterial problems. Avoid self-medication or using leftover antibiotics without medical advice.
- It is important to finish taking all antibiotics prescribed, even if you feel better, even if this means taking less. Skipping antibiotics too soon could leave bacteria undestroyed, increasing resistance against treatment.
- It is vitally important that you strictly abide by both dosage instructions and dosing protocols, especially as doing more or less than prescribed may cause ineffective treatment and negative side effects. Doing too much or too little could result in adverse consequences or may reduce effectiveness altogether.
- Do not share antibiotics It is wise to avoid sharing or taking antibiotics prescribed to other individuals; some infections require specific types of drugs, and choosing an ineffective or harmful antibiotic could prove ineffective or cause further illness.
- Avoid taking antibiotics for viral infections Antibiotics do not provide effective solutions against viral illnesses like colds and flus, but taking too many may result in antibiotic resistance and can increase their usage incorrectly.
- Inform Your Physician About Allergies and Medication Before taking any allergies or medicines, inform your physician. To reduce adverse drug interactions.
Report any adverse side effects If any unexpected side effects arise while taking antibiotics, notify your physician immediately.
Safety and Appropriate Usage of Antiseptics:
Antiseptics should only be used externally on mucous membranes, skin, or any other surfaces external to the body. You should avoid taking these treatments internally or applying them on open wounds that have an open and deep opening.
- Follow Instructions Carefully It is important to carefully read and heed any directions included with an antiseptic product as different antiseptics might require different usage instructions.
- Examine for Skin Sensitivities, Before applying antiseptic to an entire area, it is wise to conduct a small test patch on a small area of skin in order to detect any reactions or sensitivities in advance.
- Do not dilute antiseptics using water or any other substance. Diluting them could diminish their effectiveness, so this must be avoided to ensure maximum effectiveness of use.
- Store antiseptics according to their manufacturer's instructions, keeping them out of reach of children and away from direct sunlight.
- Be wary when using antiseptics; take care to avoid eye contact at all costs. Should this occur, immediately flush it out with clean water to eliminate any chance of further irritation.
- To cover all affected areas effectively and avoid skin irritation, only use enough antiseptic to cover what's necessary. Too much may result in burning sensations.
By adhering to these safety guidelines and using antiseptics and antibiotics in an ethical way, they can increase their effectiveness against diseases while at the same time helping reduce resistance to these medications. Responsible use is vital in combatting resistance as well as supporting better overall health results.
Antiseptics and Antibiotics on the basis of chemical structure
Antiseptics and antibiotics can be divided into various categories according to their chemical structures, which help determine their mechanism of action as well as their effectiveness against various microorganisms.
Here is an overview:
- Antiseptics are chemical substances designed to stop the expansion and activity of microorganisms within living tissues, typically applied topically on exterior skin surfaces such as mucous membranes and skin for cleansing purposes as well as disinfecting wounds to avoid infections or prevent them.
- Alcohols ethanol and isopropyl ethanol are widely utilized antiseptic agents due to their wide spectrum antimicrobial properties and rapid evaporation, making them perfect for fast disinfection.
- Iodine and Iodophors Iodine-based antiseptics such as povidone-iodine are proven effective at killing multiple forms of microorganisms, making them popular choices for preoperative skin preparation prior to surgery and wound care.
- Chlorhexidine is an extremely potent antiseptic with lasting antimicrobial properties, making it suitable for hand scrubs used during surgery or skin preparation prior to surgical procedures.
- Hydrogen peroxide is an antiseptic that works by releasing oxygen into the system, altering bacteria membranes and thus decreasing their growth.
- Antibiotics are highly effective medications designed to combat bacterial infections within the body. They work by targeting specific structures or functions essential to bacterial survival. Antibiotics can be divided into various categories according to both their chemical structure and mode of action
- Beta-lactam Antibiotics This class of antibiotics includes cephalosporins and penicillins with beta-lactam bands in their chemical formulae, both designed to impede bacterial cell walls and lead to their shrinking and ultimately death.
- Macrolide antibacterials such as azithromycin and erythromycin interfere with protein synthesis in bacteria cells, thus stopping the development of essential proteins necessary for survival and growth.
- Tetracyclines (Tetracycline, Tetracycline, or Tetcycines) inhibit protein synthesis by binding to cell ribosomes that produce proteins.
- Fluoroquinolones such as levofloxacin or ciprofloxacin inhibit DNA replication and repair processes within bacteria cells, leading to their death and therefore killing any chance for survival.
- Aminoglycosides like amikacin and gentamicin are aminoglycoside antibiotics, used to prevent the production of proteins by bacteria by binding with their ribosomes.
- Antiseptics offer broad protection, acting on many microorganisms including fungi, bacteria, and certain viruses; in contrast to this, antibiotics only address bacterial infections; they are ineffective against viral infections.
Antibiotics and antiseptics are essential tools in the fight against infections, so their appropriate use is vital to keeping them effective while limiting negative side effects and resistance development. Responsible use that complies with guidelines provided by healthcare providers will ensure the continued effectiveness of these vital medical drugs.
Why Topical Antiseptics Are Better for Wound Care Than Topical Antibiotics
Antiseptics designed for topical application are generally considered superior due to a number of advantages:
- Topical antibiotics feature broad-spectrum activity, which allows them to treat various microorganisms including bacteria, fungi, and certain viruses. While oral antibiotics only target bacteria specifically. Because wounds can become infected with various microorganisms easily, antibiotics provide increased protection from potential infections.
- Prevention of Resistance Antiseptics designed for topical use do not often contribute to antibiotic resistance, which occurs when bacteria become resistant to their effects and render the antibiotics ineffective. By choosing multipurpose and multiple modes of action antiseptics, your chances for developing resistant strains is reduced substantially, and this helps preserve the effectiveness of antibiotics against more serious systemic infections.
- Antiseptics have fast starting times of action, providing immediate disinfection and cleaning of wounds. Their fast action reduces bacteria load in an injured area, decreasing the risk of infection while speeding up healing time.
- Antiseptics can be easily found at pharmacies in various forms such as wipes, solutions or sprays and can easily be applied to wounds without needing a prescription or healthcare specialist; making them suitable for home use.
- Topical antiseptics tend to be cheaper than their skin-applied counterparts and offer a cost-effective option for treating minor wounds without the need for prescriptions or expensive medication.
- Antibiotics applied topically can potentially trigger allergic reactions in some individuals; however, they are generally well tolerated and carry less risk of allergic reactions or other negative side effects than oral antibiotics.
- Compatible with Wound Dressings Antiseptics are often designed to work well when combined with specific wound dressings for more effective and protective healing of wounds. This makes treatment and protection during healing faster and simpler.
- At its core, selecting topical antibiotics or antibiotics as part of wound treatment depends on both the nature and severity of an injury. For minor abrasions or cuts generally treated with topical antiseptics alone can stop the infection from spreading while encouraging healing; while more serious or infected wounds may require medical advice regarding specific antibiotics or methods that treat specific wounds.
Topical antiseptics are typically the preferred choice for wound treatment due to their broad-spectrum action and fast and effective action, along with reduced risks of antibiotic resistance. When selecting treatment for any given wound it must always take its nature and extent into account; for optimal management of these conditions always consult an experienced healthcare provider.
The Best Antiseptics and Antibiotics for Wound Treatment
Effective antibiotics and antiseptics for treating wounds depend on several factors, including the type of wound, degree of infection, and patient's medical history and allergies. Consulting medical professionals is essential to obtain an accurate diagnosis and prescription; here are a few popular and efficient antibiotics/antiseptics used for wound care.
- Antiseptics: Chlorhexidine Chlorhexidine is an effective and widely used antiseptic that is widely recognized for its broad-spectrum action against fungi, bacteria, and certain viruses.
- Povidone-Iodine: This versatile antiseptic provides multiple activities and applications. It is often employed for wound irrigation as well as skin preparation before surgery.
- Isopropyl Alcohol: This fast-acting antiseptic solution is widely used to disinfect minor cuts and cleanse skin before minor surgical procedures.
- Hydrogen Peroxide: Hydrogen peroxide contains oxygen that helps cleanse injuries quickly and effectively, making it great for cleaning small cuts or scrapes.
- Antibiotics: Bacitracin is a topical antibiotic proven to be effective against specific strains of bacteria. It is typically employed to prevent infection spread to small cuts.
- Neomycin: Neomycin can be considered another topical antibiotic and is often utilized together with polymyxin B and bacitracin in over-the-counter first-aid ointments.
- Mupirocin: Mupirocin is an antibiotic ointment designed to combat various bacteria such as Staphylococcus aureus (including MRSA). It may be used to treat impetigo as well as certain skin infections.
- Silver Sulfadiazine: Silver Sulfadiazine can be used to treat skin infections associated with burns in order to avoid or treat infection.
- Clindamycin: Clindamycin is an oral or topical antibiotic designed to fight various bacterial skin infections.
Antiseptics should only be used on minor superficial wounds, while oral or topical antibiotics are generally prescribed by doctors for more severe tissue infections or wound infections. A good wound care routine involves cleaning with antiseptics, covering with an appropriate dressing, and following medical advice to promote healing while avoiding complications.
Always consult a medical professional when treating wounds, as they will assess their unique qualities before prescribing antibiotics or antiseptics that will ensure optimal healing while also preventing infections.
Conclusion
The main difference between Antiseptics and antibiotics as well as disinfectants is that antibiotics are absorbed by the body and serve to stop and limit the development and growth of bacteria. Antiseptics operate externally within the body to stop any growth of microorganisms but don't necessarily kill them, whereas disinfectants are externally applied to non-living objects and kill bacteria.