Introduction of Dialysis and Kidney Transplant
The kidneys are essential organs that filter the excess fluids and waste from our blood. If they fail, our body is not able to effectively rid itself of these wastes, leading to serious complications.
Fortunately, medical advances provide two main lifesaving treatments for those suffering from kidney problems: dialysis as well as kidney transplants. Dialysis mimics the kidney’s function by removing the blood of waste and fluids that are not needed.
In contrast, a kidney transplant is replacing a kidney that is failing with a healthy one donated by an individual donor, with the aim of bringing back the kidney’s function. Both options have advantages, complications, and pitfalls, however, they both have the same objective of helping patients live more healthy lives.
Brief overview of kidney functions
The kidneys are bean-shaped organs that are located below the ribcage, on both sides from the back. They play an important function in maintaining our internal balance of the body and overall well-being.
Here’s a quick description of their major purposes:
- Blood Filtration: The primary role of kidneys is to eliminate toxic substances, waste products, and excess substances such as salts, water, and electrolytes from the bloodstream. These waste products are eliminated through urine.
- Regulation of fluids as well as Electrolytes: The kidneys assist in maintaining the balance of essential electrolytes such as potassium, sodium, and calcium, making sure that their levels in the bloodstream remain within an acceptable range.
- The Blood Pressure Regulation: Kidneys produce a hormone known as Renin, which helps regulate blood pressure. They make sure that the blood volume and the blood pressure remain steady.
- red Blood Cell Produced: Kidneys produce and release a hormone known as erythropoietin (EPO) as a response to low levels of oxygen in blood. EPO stimulates bone marrow, which produces greater numbers of red blood cells.
- Acid-Base Balance: The kidneys regulate the blood’s pH by either storing ousting hydrogen and bicarbonate ions making sure that the body’s internal environment remains constant.
- Metabolism of Vitamin D: Kidneys convert inactive Vitamin D from sunlight exposure and food sources into an active form known as calcitriol. It is essential for calcium absorption through the gut and bone health.
The kidneys are sophisticated machines for filtering which are constantly working to ensure that our blood is clear of harmful elements, that our electrolyte and fluid levels remain in balance, and a variety of other vital bodily functions are properly controlled. If kidneys are weak they can have wide-ranging consequences for the overall health of the body.
Explanation of chronic kidney disease (CKD) and kidney failure
Chronic Kidney Disease (CKD):
Chronic Kidney Disease often referred to as CKD is the gradual decline in kidney function as time passes. When kidneys cease their capacity to function properly and eliminate waste, the body’s waste products electrolytes, fluids, and electrolytes may build up and cause a variety of health problems.
Different stages in CKD The CKD stage is classified into 5 stages, based on the glomerular filtering rate (GFR) which is the rate at which kidneys filter blood
- stage 1. (GFR > 90 milliliters/min): Kidney damage is not severe, however, there is some evidence for kidney disease. The function is normal or elevated, however, other tests could reveal indications of damage to the kidney.
- Stage 2 (GFR 60-89 mg/min): Mild reduction in kidney function, as well as other indications of kidney damage.
- stage 3 (GFR 30 -59 mg/min): Moderate reduction in kidney function.
- Stage 4 (GFR 15-29 mg/min): Severe reduction in kidney function. Nearing kidney failure.
- stage 5 (GFR 15 mL/min): This is also known as end-stage kidney disease (ESRD) in which the kidneys have almost completely stopped working. At this point dialysis or a kidney transplant is essential to survive.
The causes of CKD:
The common causes of CKD comprise:
- Diabetes
- Hypertension of the blood vessels (hypertension)
- Glomerulonephritis (inflammation of kidney’s units for filtering)
- Polycystic kidney disease
- Prolonged urinary tract infections
- Recurrent kidney infections
Kidney Failure:
Kidney failure, also known as “end-stage renal disease” (ESRD) as described above can be described as the advanced form of CKD. At this point, the kidneys function at less than 10 percent of their capacity.
Types of Kidney Failure:
- Acute Kidney Injuries (AKI): This is a sudden and brief impairment of the kidneys that can be caused by an extreme illness, certain medication trauma, or a decrease in circulation of blood to the kidneys. Certain patients can be able to recover from AKI by taking appropriate care, however, others may be diagnosed with CKD.
- Chronic Kidney Failure It is a permanent and irreparable decline in kidney function over time that leads to the build-up of waste products, toxins, and excessive fluids within the body.
The signs of kidney failure: As the kidneys become dysfunctional, various symptoms could manifest, including:
- The feet, hands, and on the face
- The weakness and fatigue of the body
- Breathing shortness
- Nausea and vomiting
- Heart rhythms that are irregular or chest pain
- Changes in the output of urine
- Mental confusion
- Seizures come in the most severe instances
The treatment for kidney failure: When a person develops the point of kidney disease, they will require kidney replacement therapy to live. The two most common treatments are:
- Dialysis: It mimics kidneys by eliminating waste products and excess fluids from the blood.
- Kidney Transplantation: Surgically replacing the damaged kidney with a healthy one from the donor.
CKD is a condition that progresses which causes the decline of kidney function. If left untreated or treated correctly, it could result in kidney failure that requires life-saving procedures such as dialysis and transplantation. Proper treatment, lifestyle modifications as well as regular check-ups may aid in the treatment of the illness.
What is Dialysis?
Dialysis is a procedure that mimics normal kidney functions in cases where one’s kidneys are unable to be effective in their work. It’s a life-support procedure that purifies and filters blood with an instrument. This aids in maintaining the balance of minerals and salts and helps eliminate fluid and waste. Dialysis is usually used by those suffering from kidney failure. often referred to as end-stage renal disorder (ESRD).
Types of Dialysis:
- Hemodialysis (HD):
-
- Description and procedure: Hemodialysis is the most commonly used kind of dialysis. It is a process where the blood is removed from the body of the patient through a dialyzer. It is also called the “artificial kidney.” The dialyzer is used to eliminate the toxins, waste, and fluids that are not needed, and the cleansed blood is delivered back into the body.
- Access: Prior to being able to start hemodialysis, there must be a method to gain access to the blood via an access vascular or surgically-created vein that is which is used to take out and replenish blood during treatment. The three kinds of vascular access used to be used for hemodialysis that lasts a long time are arteriovenous (AV) fistula as well as AV grafts and a venous cath.
- Time of operation: In general, treatments for hemodialysis are planned three times per week. They can last between 3 to 5 hours each time, based on the individual’s needs and the type of dialysis machine that is used.
- Peritoneal Dialysis (PD):
-
- Description and method: Peritoneal dialysis uses the abdominal cavities (the peritoneum) as a filtering system to eliminate waste and excess fluid out of the human body. The catheter can be surgically placed in the abdomen, and dialysis solutions are replenished and then drained several times per day. When the solution is placed within the abdominal cavity, it removes excess fluid and wastes from the blood.
- The types of dialysis: There are two main kinds of peritoneal dialysis Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD or CCPD). CAPD does not require a device and exchanges are conducted by hand several times per day. APD makes use of an instrument (cycler) for multiple exchanges in the evening as the patient is asleep.
- Time: The frequency and duration of the HTML0 vary depending on the kind of PD and the medical condition of the patient. For example, CAPD usually requires exchanges every 4-6 hours while APD is a nighttime condition that requires exchanges at night.
Advantages of Dialysis:
- A quick and effective solution for those suffering from kidney failure, particularly those who are waiting for transplants isn’t an option.
- Provides a degree of flexibility in routines of daily life, especially when using peritoneal dialysis.
- Dialysis is a treatment that can enhance the quality of life and extend the duration of life.
Disadvantages/Complications:
- This can take a lot of time and need significant lifestyle changes.
- The potential risks are infections Low blood pressure muscle cramps, as well as excessive fluid.
- Dialysis for long periods can cause various health issues, including peritoneal membrane dysfunction (for PD), vascular access issues (for HD), and other health issues that are chronic.

Dialysis is an important treatment option for those suffering from kidney problems, providing the ability to control their condition and ensure the appearance of normality within their lives. Determining between hemodialysis and peritoneal dialysis is often based on the individual’s health condition as well as lifestyle and preferences.
What is Kidney Transplant?
An organ transplantation is an operation in which the healthy kidney of an individual donor is transplanted into the kidney of a patient whose own has failed. The new kidney assumes the responsibility of purifying and filtering the blood, thereby returning the balance of the body’s electrolytes and fluids. It can be a substitute for dialysis for patients suffering from End-stage renal disease (ESRD) or chronic kidney disease.
Sources of Donor Kidneys:
- Living Donors:
-
- Most often, it is a family member, a friend, or, sometimes, an unknown person.
- One kidney is the best option since humans can live in a healthy way by having just one kidney functioning.
- It requires a thorough assessment process to determine the compatibility and health of the donor.
- Deceased Donors:
-
- People who have passed away, usually suddenly, from accidents, however, whose kidneys are functional.
- Organ allocation is usually determined by waiting time and medical urgency, organ size, blood, and tissue type compatibility, as well as geographical area.
Transplant Process:
- Pre-transplant evaluation: Candidates undergo a thorough evaluation to determine if they’re suitable to undergo a transplant, taking into consideration their general health, potential risks, as well as advantages.
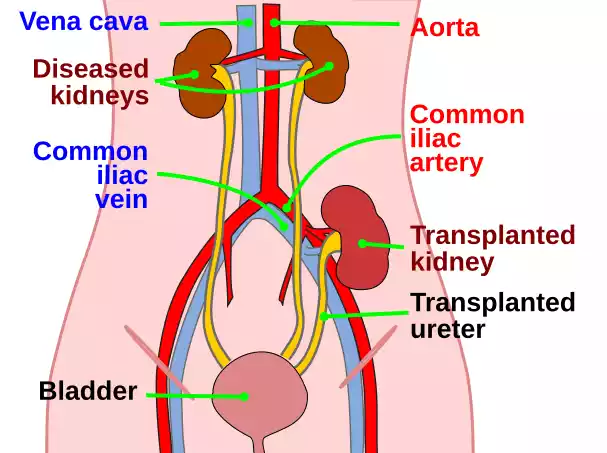
- Operation Procedure: A kidney that is not functioning is typically left in place until it causes problems. The kidney transplanted is surgically placed into the abdomen’s lower part. Blood vessels from the kidney that are transplanted are connected to blood vessels located in the lower portion of the abdomen. the ureter of the kidney that is transplanted is connected to the bladder.
- Post-surgery Treatment and Monitoring: After surgery, patients are monitored closely to ensure that the newly created kidney is working properly and there aren’t any complications. Modifications to medications, specifically immunosuppressive medications, are typical during this time.
Post-transplant Medication and Care:
- Immunosuppressive Drugs: These are drugs that aid in preventing your body’s immune system from attacking and destroying the kidney transplant. Although they are essential to ensure longevity after the procedure, they may cause side effects and make patients more prone to infections.
- Routine Check-ups: regular visits with a transplant doctor to check that the kidney is working well and that there is no evidence of rejection or any other complications.
Advantages of Kidney Transplant:
- Longer-lasting results in transplants that are successful compared to long-term dialysis.
- There are fewer restrictions on fluids and diet than dialysis.
Complications and Risks:
- The rejection of the Kidney that is New: The body’s immune system could recognize mymedic.es the kidney’s foreignness and may attempt to target it.
- Diseases: The use of immunosuppressive medicines can reduce your immune system which makes the patient more vulnerable.
- Drugs’ effects: Some drugs may produce side effects like weight gain, bone loss, or an increased susceptibility to certain cancers.
- Potential Recurrences of Initial Kidney Disease: Some kidney diseases could recur when the kidney is transplanted.
A kidney transplant can be an extremely life-changing option for people suffering from kidney disease. It gives the possibility of an almost normal life, but it has its own challenges like the requirement to take life-long medication as well as the potential for complications. However, a lot of recipients of kidney transplants live full, healthy lives.
Dialysis and Kidney Transplant in the comparison chart
| Aspect | Dialysis | Kidney Transplant |
|---|---|---|
| Definition | A procedure that replicates kidney functions by purifying and filtering blood using a machine. | A surgical procedure to implant a healthy kidney from a donor into a person with kidney failure. |
| Purpose | To remove waste, and excess fluid, and balance electrolytes in the absence of functional kidneys. | To replace the non-functional kidneys and restore typical kidney functions. |
| Duration/Frequency | Ongoing and regular. Hemodialysis typically 3 times a week; Peritoneal dialysis may be daily. | Once successful, no need for repeated procedures unless the transplant fails. |
| Life Expectancy | Generally, transplant patients have a longer life expectancy compared to long-term dialysis patients. | Typically offers a longer life expectancy compared to long-term dialysis. |
| Quality of Life | May experience limitations due to treatment schedules, dietary restrictions, and physical effects. | Generally improved quality of life, with fewer restrictions post-recovery. |
| Cost | Ongoing cost due to regular sessions and related medications. | Initial cost for the surgery, followed by costs for post-surgical care and lifelong medications. |
| Procedure Type | Non-surgical (though access points may require minor surgery). | Surgical. |
| Primary Risks/Complications | Infections at access points, low blood pressure, muscle cramps, fluid overload, long-term effects on heart and bones. | Rejection of the new kidney, effects of immunosuppressive drugs, surgical complications, recurrence of original kidney disease. |
| Maintenance | Requires consistent adherence to schedule and potential dietary and fluid restrictions. | Requires lifelong medications (especially immunosuppressants) and regular medical check-ups. |
| Availability | Widely available and can start immediately once the patient is deemed eligible. | Depending on the availability of a matching donor; may involve waiting periods. |
It’s crucial to note that the best treatment option between dialysis and kidney transplant varies based on individual circumstances, including health status, age, availability of donors, and personal preferences. Consulting with a nephrologist and transplant specialist is essential for making an informed decision.
What are the similarities between Dialysis and Kidney Transplant?
- Principal Goal: Both dialysis and kidney transplants seek to fill or substitute for the functions of kidneys that are failing. They aid in the elimination of the body of waste products, remove excess fluids, and regulate electrolytes in the body.
- Life-Saving Methods: Both treatments can save lives for people suffering from End-Stage Renal Disease (ESRD) as well as severe kidney problems.
- Medical Supervision: Both require constant and comprehensive medical supervision. Dialysis patients are regularly seen in dialysis centers, and transplant recipients undergo regular check-ups to check kidney function and any potential complications.
- Long-term medical intervention: Both treatments are not one-time solutions. Dialysis is an ongoing process and transplant recipients need continuous monitoring and medications.
- Risk of complications: Both treatments come with a risk. Dialysis could cause complications with cardiovascular disease, infections, and other issues, while transplant recipients may be at risk of rejection of organs, the side negative effects of immunosuppressant medication as well as the potential for recurrence of the kidney disease that caused them originally.
- Immediate Considerations for Immunology: Hemodialysis patients might have reactions to the contact of blood with membranes from dialysis transplant recipients and may require immune-suppressive medications to avoid rejection of organs.
- Lifestyle and dietary Concerns: Patients from both categories typically receive guidance or instructions regarding lifestyle choices and dietary restrictions or fluid intake, particularly during the first few days after beginning treatment or after transplant.
- Cost implications: Both dialysis and kidney transplants are costly. However, the nature of costs is different (ongoing dialysis, and the initial and long-term expenses for transplants) the financial aspect plays an important role in the treatment choices in a variety of healthcare systems.
- Psychology Impact: Dialysis, as well as transplants, can have profound emotional and psychological effects on patients, impacting their overall quality of life and psychological well-being in addition to social relationships.
- Training and preparation: Prior to undergoing any procedure, patients are informed about the procedure, possible dangers, benefits, and lifestyle changes they could require.
Making an Informed Decision
If you are confronted with a condition that is advanced, such as kidney illness or end-stage renal disease (ESRD) having to choose between dialysis or transplantation of the kidney can be difficult. Making an informed decision requires knowing the advantages, risks, and implications of each option, as well as taking into consideration your personal situation and personal preferences.
Here’s a reference to help you make this choice procedure:
Medical Evaluation:
- Participate in a comprehensive medical assessment to assess the condition in your renal function and overall condition as well as any comorbid conditions.
- This will allow you to determine whether you’re a good candidate for transplantation, or if dialysis is a more urgent or suitable alternative.
Understand the Procedures:
- Be aware of the procedure involved as well as the associated risks as well as the potential benefits and the problems.
- Ask questions regarding how often, the duration, and the invasiveness of treatment.
Consider Quality of Life:
- Take a look at the way each treatment plan will work with your current lifestyle.
- If it’s successful, a transplant may provide greater freedom and fewer limitations than dialysis. Waiting in search of a compatible donor may be lengthy and requires an ongoing commitment to medication and subsequent follow-ups.
Lifespan and Prognosis:
- Think about the lifespan that could be provided by every treatment. While a successful transplant of the kidney will result in a greater life expectancy than dialysis for long-term use There aren’t any guarantees.
- Be aware of the possibility of problems or the necessity to repeat procedures in the near future.
Financial Implications:
- Consider the cost associated with each choice including the insurance coverage, expenses out of pocket as well as long-term medical expenses.
- Be aware of the indirect costs too like time off from work, transport in order to attend medical appointments, or modifications to the way you live.
Emotional and Psychological Aspects:
- Think about how each treatment can affect your mental as well as emotional health.
- Find support groups or counseling for discussion of fears, worries, and anxieties. Sharing your experiences with other people who have faced similar situations may provide useful insight.
Talk to Multi-Experts
- Alongside your primary nephrologist, think about getting second opinions.
- Meet with dialysis teams, transplant teams, specialists, or even patients who have undergone dialysis procedures to gain a variety of perspectives.
Support System:
- Explore your options with family members and close friends. Their perspectives, opinions, and opinions can prove valuable in deciding.
- Think about the role they’ll play in your treatment for transport to dialysis sessions and post-transplant treatments, or even emotional assistance.
Stay Updated:
- Medical advancements are often occurring. Be aware of new technologies, treatments, and research that may affect your choice.
Trust Your Instincts:
- While expert and data-driven opinions are important, your personal sense of comfort and sensitivity have a major role to play. Consider what is comfortable for you. Think about your personal objectives and values as a person.
making the decision between dialysis or a kidney transplant is a major decision that requires careful evaluation of many aspects. Work with your healthcare providers lean on your family and friends and be sure to take the time to choose a path that is best suited to your needs in terms of health and objectives.
Conclusion
The decision to choose between dialysis and a kidney transplant is an important decision to make when managing kidney disease that is advanced. Both choices have advantages, disadvantages, and ramifications.
It is essential to stay informed, consult with experts take into account personal circumstances, and put the highest priority on one’s quality of life and overall well-being. With the right information and guidance, the individual can select the path that is most in line with their health goals and aspirations for life.