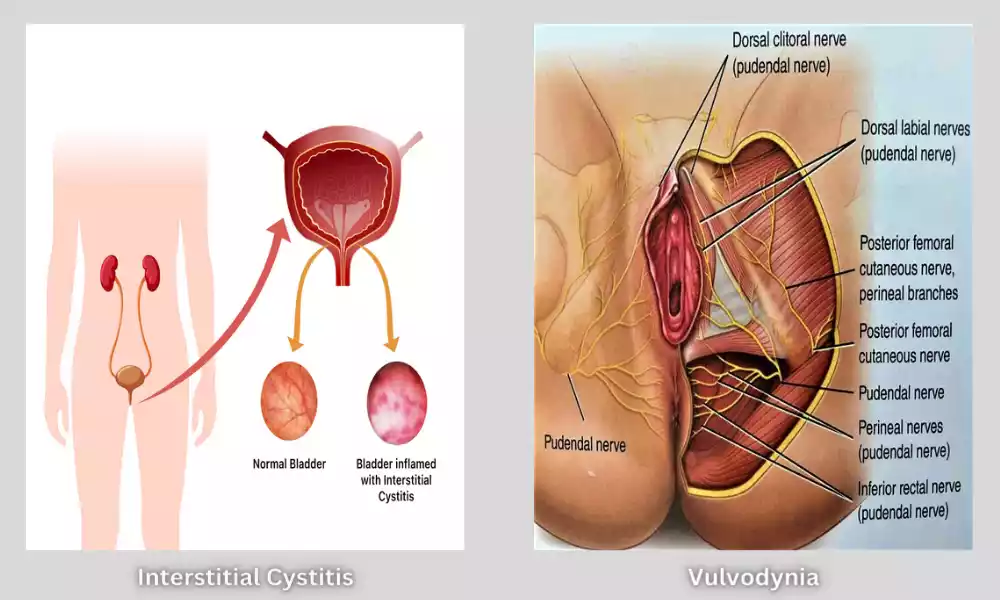
Interstitial Cystitis and Vulvodynia, two chronic pain conditions that primarily affect women, are often overlapping but distinct. IC is characterized by chronic bladder inflammation and discomfort, which can lead to frequent urination.
Vulvodynia causes pain when sexing or sitting. Both conditions are difficult to manage and require specialized treatment for better quality of life and symptom management.
What is Interstitial Cystitis (IC)
Interstitial Cystitis, also known as Painful Bladder Syndrome (PBS), is a chronic condition that primarily impacts the bladder. It is characterized as:
- Pelvic pain: People with IC often experience severe and persistent pelvic pain.
- Urinary Urgency Increased: Urinary urgency is increased, resulting in frequent bathroom visits.
- Urinary Frequency Increased: People who have IC may urinate more often than normal, even at night. This can disturb sleep.
- Urination Can Be Painful: Urinating can be painful for those with IC. They may feel a burning sensation or discomfort.
- Small Urine Quantities: Despite frequent urges to urinate only small quantities of urine can be passed at each occasion.
- No infection: Infection is not the cause of IC, even though it can have symptoms that are similar to those associated with a urinary system infection (UTI).
It is still not known what causes IC, but a number of factors are believed to be involved, such as bladder inflammation, a defect in the bladder lining that protects it, and an excessive immune response. The diagnosis often requires ruling out other possible causes of the symptoms.
IC can have a significant impact on a person’s life. Treatment options may include bladder installation, physical therapy, medications that reduce pain and inflammation, dietary changes and a variety of other treatments. In severe cases, surgery is an option. Management strategies are customized to each individual and are designed to reduce symptoms and improve well-being.
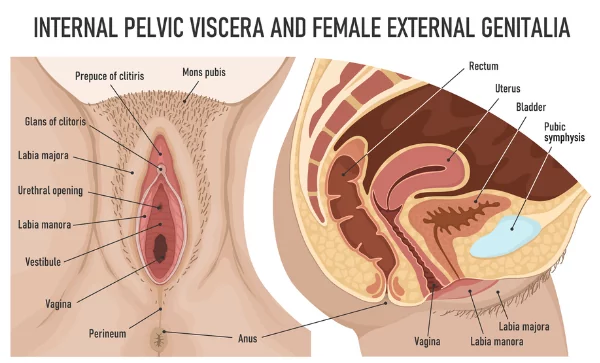
What is Vulvodynia?
Vulvodynia, also known as chronic pain, is a condition that affects primarily the vulvar region. This includes the external female genitalia. The condition is characterized as persistent and unexplained discomfort or pain in the vulva. It can be localized, or it can be diffuse.
Vulvodynia is characterized by:
- Pain: People with vulvodynia may experience a variety of types of pain including burning, stinging or aching in the vulvar area.
- Chronic nature: The condition of vulvodynia can be chronic because it lasts more than three months and may persist for many years.
- Unprovoked and Provoked Pain: Pain can be caused by sexual activity, tampon use, prolonged sitting, or other activities that put pressure on the vulva. Unprovoked pain can also happen spontaneously, without any obvious trigger.
- Impact of Vulvodynia on Quality of Life: The pain caused by vulvodynia may have a significant impact on a person’s daily activities, sexual function and emotional well-being.
It is still not known what causes vulvodynia. However, it is thought to be a combination of factors including nerve dysfunctions, inflammation, abnormal muscle movements, and hormonal fluctuations. The diagnosis involves a complete medical evaluation in order to rule out any other possible causes of vulvar discomfort, such as skin conditions or infections.
The treatment for vulvodynia can be individualized and may include different approaches such as topical medication, physical therapy or nerve blocks, dietary changes, and counseling. Treatment aims to improve the overall comfort and well-being of the patient by managing symptoms. Vulvodynia can be a difficult condition to manage, and it is important that healthcare providers provide ongoing support.
What are the Symptoms of Vulvodynia
Vulvodynia causes persistent pain in the vulvar region. Symptoms can vary, but they include:
- Burning Feeling: Many women who suffer from vulvodynia report a burning sensation or stinging in the vulvar area. This discomfort can range from mild up to severe.
- Soreness or Rawness: Some people experience soreness or rawness in their vulva. This can make wearing tight clothes or sitting for long periods of time uncomfortable.
- Shooting or Stabbing Pain: Vulvodynia may also present as sharp or stabbing pains in the genital region.
- Itching Although less common, itching can be a sign of vulvodynia.
- Dyspareunia (Pain During Sexual Intercourse): Many women who have vulvodynia experience pain during sexual activity and may feel discomfort afterward.
- Tampon Pain: For some women with vulvodynia, inserting tampons and undergoing gynecological exams can be painful.
- Hypersensitivity: Even a gentle touch can be painful.
- Chronic Pain: The pain that persists over a long period of time, usually three months or longer, is considered chronic.
- Pain while Resting: Vulvodynia can cause pain when no obvious trigger is present, for example, during rest or sitting.
Individuals’ severity of symptoms may differ. Others may suffer from intermittent symptoms, while some individuals experience constant discomfort. The pain caused by vulvodynia may have an impact on the quality of life for a patient, as it can affect their daily activities, emotional health, and intimate relationships.
It is vital that you consult a doctor who is a specialist in women’s healthcare or vulvar discomfort to diagnose the condition and discuss treatment options.
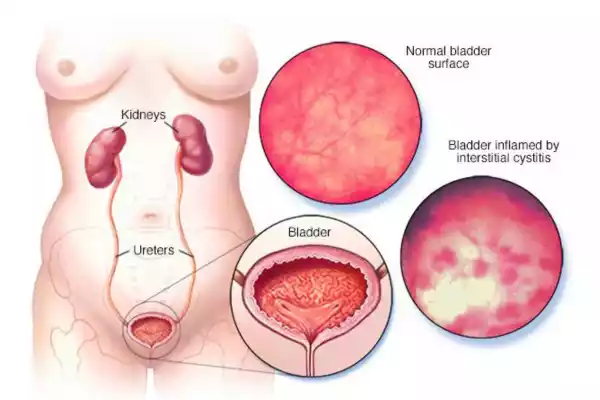
What are the Symptoms of Interstitial Cystitis?
Interstitial Cystitis (IC), also known as Painful Bladder Syndrome, is characterized by a range of symptoms primarily related to the bladder and pelvic region.
The symptoms of IC can vary from person to person and may include:
- Pelvic Pain: Chronic and often severe pain in the lower abdomen and pelvic area is a hallmark symptom of IC. The pain can be constant or intermittent, and its intensity may vary.
- Increased Urinary Urgency: Individuals with IC often have a strong, frequent urge to urinate, even when the bladder is not full. This sense of urgency can be distressing.
- Increased Urinary Frequency: Frequent urination is a common symptom, with some people needing to urinate as often as 60 times a day. This can significantly disrupt daily activities and sleep.
- Painful Urination (Dysuria): Voiding the bladder can be painful or uncomfortable, and some people with IC experience a burning sensation during urination.
- Small Urine Volumes: Despite the frequent urge to urinate, only small amounts of urine may be passed each time.
- Nocturia: Frequent nighttime urination can disturb sleep patterns.
- Painful Sexual Intercourse: IC-related pelvic pain can make sexual intercourse painful or uncomfortable for some individuals.
- Bladder Pressure or Fullness: Some people with IC may feel a constant sensation of bladder pressure or fullness.
It’s important to note that IC symptoms can mimic those of a urinary tract infection (UTI), but unlike a UTI, IC is not caused by bacterial infection. The exact cause of IC is not fully understood, but it is believed to involve a combination of factors, including bladder inflammation, defects in the protective bladder lining, and an overactive immune response.
Diagnosis of IC typically involves a thorough medical evaluation to rule out other possible causes of these symptoms. Treatment for IC is tailored to the individual and may include dietary modifications, medications to reduce inflammation and pain, bladder instillations, physical therapy, and in some cases, surgical interventions. The goal of treatment is to alleviate symptoms and improve the patient’s quality of life.
Interstitial Cystitis and Vulvodynia in the comparison chart
Certainly, here is a comparison chart highlighting some key differences and similarities between Interstitial Cystitis (IC) and Vulvodynia:
| Aspect | Interstitial Cystitis (IC) | Vulvodynia |
| Primary Location | Bladder | Vulvar region |
| Main Symptom | Pelvic pain, urinary symptoms | Vulvar pain, discomfort |
| Pain Type | Pelvic pain, burning sensation | Burning, stabbing, aching, rawness |
| Urinary Symptoms | Frequent urination, urgency, dysuria | None (unless concurrent UTI) |
| Pain Triggers | Full bladder, certain foods, stress | Sexual intercourse, tampon use, prolonged sitting |
| Sexual Discomfort | Possible, due to pelvic pain | Often painful or impossible due to vulvar pain |
| Diagnostic Process | Ruling out other causes of pelvic pain | Ruling out other vulvar conditions |
| Possible Causes | Bladder inflammation, immune response | Nerve dysfunction, muscle abnormalities, hormonal changes |
| Treatment Approaches | Dietary changes, medications, instillations, physical therapy | Topical medications, physical therapy, nerve blocks, dietary changes |
| Chronic Nature | Chronic condition | Chronic condition |
| Impact on Quality of Life | Can be significant, affecting daily activities | Can be significant, affecting daily activities and sexual function |
| Prevalence | More common in women | More common in women |
Please note that while these are common characteristics of IC and Vulvodynia, individual experiences may vary, and the presentation of symptoms can differ from person to person. It’s essential for individuals experiencing these symptoms to consult with healthcare professionals for accurate diagnosis and appropriate management.
Importance of distinguishing between IC and Vulvodynia
It is important to distinguish between Interstitial Cystitis and Vulvodynia for several reasons:
- Appropriate treatment: Vulvodynia and IC are two distinct conditions, with different causes and treatments. A misdiagnosis of the two conditions can lead to an inappropriate treatment that may not alleviate symptoms and improve the patient’s quality of life. A precise diagnosis allows for tailored treatments that target the specific condition.
- Avoiding Ineffective Procedures: A misdiagnosis may lead to medical procedures that are not necessary, such as surgery, and which could be harmful to the patient. Correct differentiation can help avoid unnecessary invasive interventions.
- Effective Symptom Management: Both IC and Vulvodynia may have a significant effect on a person’s well-being and daily life. A correct diagnosis allows healthcare providers to prescribe the appropriate medications, therapies, and lifestyle changes in order to manage symptoms effectively and improve patient comfort and quality.
- Emotional Impact: These conditions can lead to emotional distress, and have a negative impact on mental health. A correct diagnosis allows healthcare professionals to offer emotional support, counseling, and resources that are tailored to each condition. This helps patients better cope with their circumstances.
- Improving the Quality of Life: By identifying ICs from Vulvodynia, healthcare providers can create individualized and comprehensive management plans that address the root causes of each condition. This can improve symptom control and comfort for patients, as well as their overall quality of life.
- Avoiding unnecessary costs: A misdiagnosis can lead to a lot of doctor visits, tests, and treatments that may not work. By streamlining the healthcare process, accurate diagnosis can save time and money for patients.
- Promote Understanding: A clear differentiation between IC, Vulvodynia, and other conditions can help patients, their families, and others better understand the condition, the causes, and appropriate management strategies. This can help reduce the anxiety and uncertainty that surrounds this condition.
It is important to distinguish between Interstitial Cystitis (IC) and Vulvodynia (VD) to ensure individuals receive the correct diagnosis, appropriate treatment, and support needed to effectively manage their condition. It not only helps to control symptoms, but it also improves the quality of their life and overall health.
Similarities Between IC and Vulvodynia
Interstitial Cystitis and Vulvodynia, although distinct medical conditions share many similarities:
- Chronic pain: Both IC (incontinence) and Vulvodynia (vulvar pain) cause chronic pelvic-regional discomfort. Although the location and type may vary (bladder in IC, and vulvar in Vulvodynia), both conditions cause long-lasting pain.
- Impact on Quality of Life: These conditions can have a significant impact on a person’s life quality. Chronic pain caused by IC or Vulvodynia may interfere with everyday activities such as work, social interaction, and intimate relationships.
- Gender predominance: Vulvodynia and IC are more common in women than men, but they can affect anyone.
- Diagnosis by Exclusion: These conditions are diagnosed using a process called exclusion. Before diagnosing IC or Vulvodynia, healthcare providers usually rule out any other possible causes.
- Multidisciplinary care: The management of these conditions is often best achieved by a multidisciplinary team. Healthcare providers with different specialties such as urologists and gynecologists may be involved in treating individuals with IC.
- Impact on Patients: Both IC and Vulvodynia, can have an emotional and psychological impact on patients. Chronic pain can cause anxiety, depression, and emotional distress.
- Overlapping Symptoms: Some people may experience symptoms that overlap IC and Vulvodynia. Vulvodynia, for example, can cause pelvic pain that is similar to IC symptoms.
- Management strategies: Although the treatment for IC is different from that of Vulvodynia due to the differences in the affected areas (bladder vs. vulva), there may be some complementary strategies such as dietary changes, physical therapy, and pain management techniques.
Despite their similarities, it is important to understand that IC and Vulvodynia represent separate conditions. They have distinct causes and require different treatment methods. It is important that healthcare providers differentiate and diagnose patients correctly to develop management plans that are tailored to their individual needs.
Misdiagnosis and Coexistence
The misdiagnosis of medical conditions and the coexistence of other conditions can make it difficult to understand and manage chronic pain conditions such as Interstitial Cystitis and Vulvodynia.
These factors are important to consider:
- Misdiagnosis:
-
- IC & Vulvodynia: A misdiagnosis may occur when symptoms of IC / Vulvodynia or other conditions are mistaken. The pain and symptoms of IC could be mistaken for a UTI or an overactive bladder. This would lead to the wrong treatment.
- Misdiagnosis Impact: A misdiagnosis may lead to unnecessary medical procedures and delays, as well as frustration on the part of the patient. This can lead to the use of ineffective medications and treatments that don’t address the underlying problem.
- Coexistence Conditions:
-
- IC & Vulvodynia: Certain individuals may experience both IC & Vulvodynia at the same time. It can be difficult to diagnose because pain from one condition can exacerbate symptoms of another. Vulvodynia, for example, can cause bladder pain that is related to IC.
- Management Challenges: Managing IC and Vulvodynia coexisting can be difficult due to the necessity to address symptoms associated with both conditions. To develop a comprehensive plan of treatment, healthcare providers must evaluate and differentiate the symptoms of each condition.
- Overlapping symptoms:
-
- Symptoms that overlap: IC, Vulvodynia, and other conditions may have some symptoms in common, including pelvic pain, urgency, and frequency of urination.
- Need for Comprehensive Evaluation: When symptoms overlap, it is important to conduct a thorough evaluation that includes a medical history, physical exam, and possible diagnostic tests. This will help diagnose the condition and distinguish between them.
- Multidisciplinary approach:
-
- Effective management: Due to the complexity of IC and Vulvodynia as well as misdiagnosis and coexistence, a comprehensive approach involving specialists from urology and gynecology along with pain management and other relevant fields is often necessary.
- Patient Advocate: Individuals with chronic pain should advocate for themselves, and seek a second opinion if they believe that their symptoms have not been adequately addressed by the healthcare provider.
Misdiagnosis, as well as the coexistence of multiple conditions, can make it difficult to manage chronic pain conditions such as IC or Vulvodynia. To ensure accurate diagnosis and treatment, it is important to have clear communication with your healthcare provider, seek specialized care if needed, and conduct a thorough evaluation.
Diagnosis of Interstitial Cystitis and Vulvodynia
The diagnosis of Interstitial Cystitis and Vulvodynia is a thorough evaluation performed by healthcare professionals who are usually specialists in urology, gynecology, or both.
Here are some general diagnostic and treatment considerations for each condition:
Diagnosis for Interstitial Cystitis:
- Medical history: Healthcare professionals will begin by taking a medical history. This includes information on the patient’s symptomatology, the duration of the symptoms, and any factors which may exacerbate or relieve the symptoms.
- Physical Exam: You may perform a physical exam including a pelvic examination to look for signs of infection and other conditions that can mimic IC.
- Urinalysis & Culture: Urinalysis & culture are commonly performed to rule out urinary infections (UTIs) that can have similar symptoms.
- Cystoscopy: This procedure is a critical diagnostic tool for IC. The bladder lining is directly visible with the cystoscope. During cystoscopy, healthcare providers can also perform a bladder biopsy to assess for signs of IC and inflammation.
- Potassium-Sensitivity Test: Injecting a potassium chloride solution into the bladder will trigger pain that is indicative of IC.
- Urodynamic Tests: In certain cases, urodynamic testing may be performed in order to assess bladder function. This includes pressure measurements when the bladder is filled and emptied.
- Pelvic Imaging: In some cases, imaging tests like CT scans or MRI can be used to rule out other conditions or complications associated with IC.
Diagnosis for Vulvodynia :
- Medical history: Just as with IC, obtaining a medical history in detail is the first thing to do. Included in this discussion are symptoms, pain characteristics, and any factors that may trigger or relieve the pain.
- Physical Exam: The pelvic area is examined carefully to look for signs of skin conditions and inflammation.
- Pain Maps: Healthcare professionals may use pain mapping to pinpoint the location and symptoms of pain.
- Biopsy: A biopsy of vulvar tissue is sometimes performed to confirm a diagnosis and rule out any other condition.
- Cotton Swab Test: The test involves gently pressing a cotton swab on specific areas in the vulvar area to determine pain sensitivity.
- Vaginal culture: In order to rule out infection, vaginal cultures can be performed in order to check for yeast and bacterial overgrowth.
- Neurological Assessment: An assessment of the nerves within the vulvar region can be conducted to determine the function.
Both IC and Vulvodynia fall under the category of conditions of exclusion. This means that any other possible causes of symptoms must be ruled out prior to a diagnosis being confirmed. Diagnostic tests for these conditions may be complicated and involve consultations with experts and multiple tests.
If you or a loved one is experiencing symptoms of IC, Vulvodynia, it’s important to seek out a healthcare professional with experience in this condition. This will allow for a more accurate diagnosis and explore the best treatment options.
Conclusion
Interstitial Cystitis and Vulvodynia, two chronic pain conditions affecting primarily women, are often difficult to treat. It is important to have a proper diagnosis that includes a thorough evaluation in order to distinguish between these conditions and possible causes of similar symptoms.
The first step to developing a treatment plan that is tailored to each individual’s needs and ultimately improves their quality of living and well-being is an accurate diagnosis.