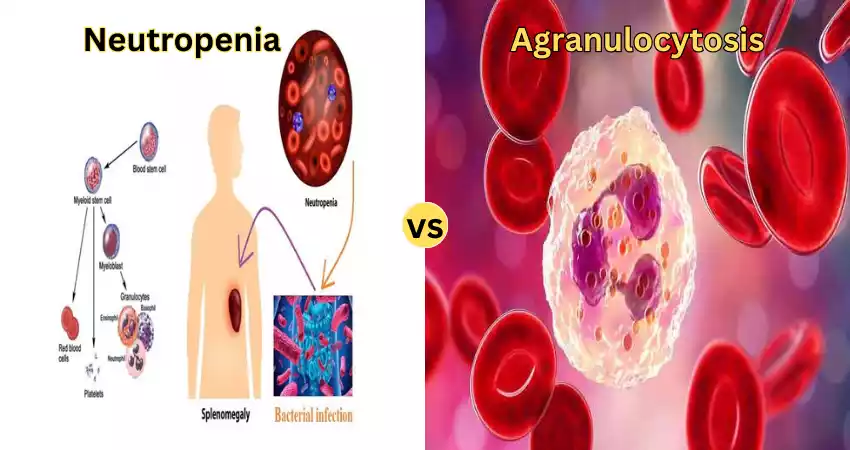
The primary distinction between agranulocytosis and neutropenia is that neutropenia occurs when an individual has a lower amount of neutrophils in their bloodstream and agranulocytosis occurs the case when a person has low levels of granulocytes.
These include basophils, neutrophils, and eosinophils, in their circulating blood. Neutropenia and agranulocytosis are two conditions caused by low levels of specific white blood cells. Granulocytes are a kind of white blood cell with tiny granules inside them.
The three types of granulocytes found in humans include eosinophils, neutrophils, and basophils. Agranulocytosis can be called the most severe form of neutropenia because in this case, the level of neutrophils drops to below 100 microlitres of blood.
What is agranulocytosis?
Agranulocytosis (pronounced “ay-GRAN-yoo-loh-sy-TOH-sis”) is a life-threatening condition that involves having severely low levels of white blood cells called neutrophils. White blood cells make up an integral part of the immune system. They shield your body from infections by fighting against germs that can make you sick.
Insufficient levels of neutrophils make people more susceptible to infection. It is possible to contract germs that aren’t hazardous otherwise. Agranulocytosis is the name given to it by “granulocyte.” Granulocytes are white blood cells that have enzymes that kill germs as well as break down substances that can damage the body.
There are three kinds of granulocytes, namely neutrophils basophils, and eosinophils. The majority of the white blood cells in your body are neutrophils. This is the reason why health professionals examine the levels of neutrophils in order to diagnose agranulocytosis.
What is neutropenia?
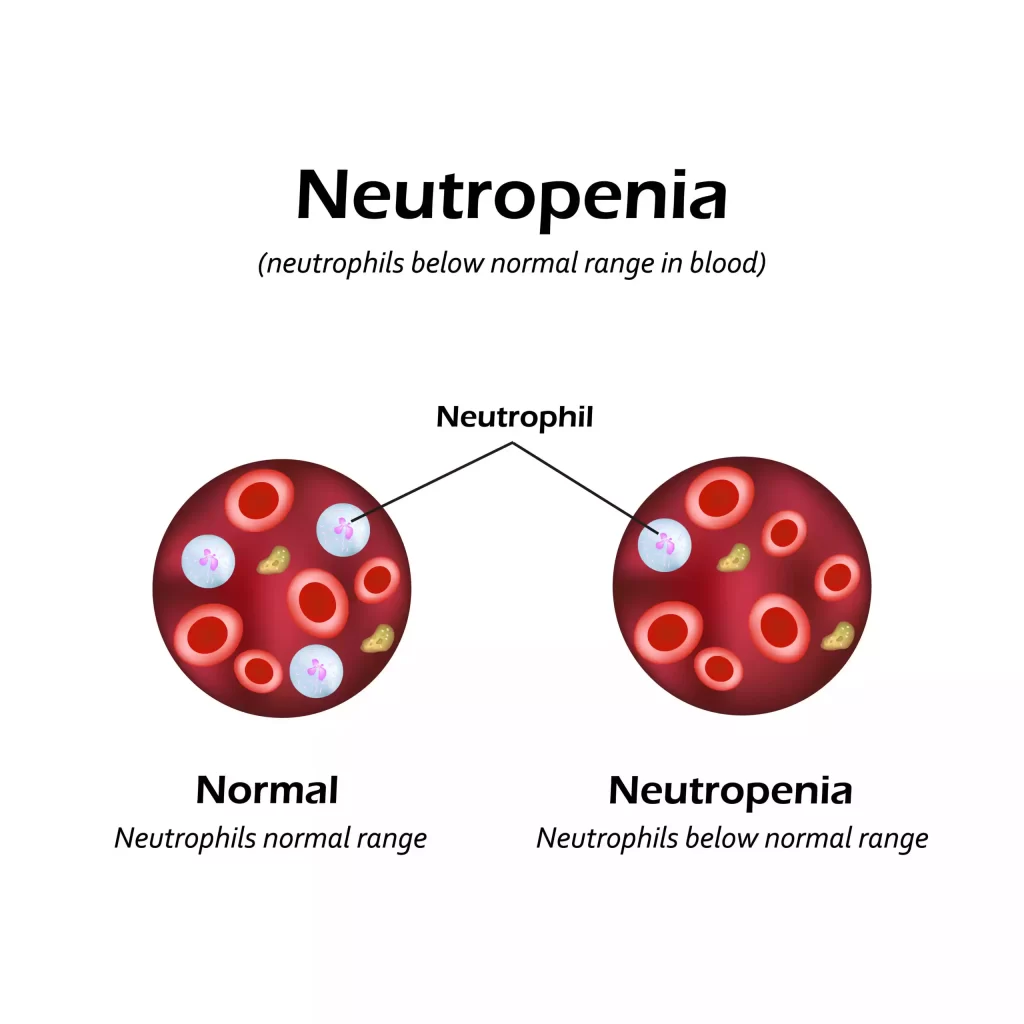
Neutropenia (noo-troh-PEE-nee-uh) refers to lower-than-normal levels of neutrophils in your blood. A neutrophil is a form of white blood cell that the bone marrow produces most of white blood cells, in general, and specifically neutrophils combat infections in your body. Neutrophils eliminate bacteria that cause infections like bacteria and viruses.
Lacking enough neutrophils makes it more difficult for your body to fight against germs and keep infections at bay. In extreme cases, the bacteria your body is accustomed to (like the bacteria that reside in your mouth and your intestines) could cause illness.
Types of Agranulocytosis
There are two categories of agranulocytosis.
- Inherited: Agranulocytosis (IAGC) is caused by a genetic condition that impacts your body’s production of neutrophils. This form is more likely to occur among babies and children.
- Acquired: Agranulocytosis has many possible sources, but medication side effects account for approximately 70% of cases of acquired Agranulocytosis cases. Adults tend to suffer more commonly from acquired agranulocytosis.
Types of Neutropenia
Neutropenia can be broken down into four major types.
These are:
CONGENITAL NEUTROPENIA
Sometimes referred to as Kostmann Syndrome, congenital neutropenia typically manifests itself at birth and often shows significant severity due to neutrophils being completely absent.
Patients typically display what’s known as “maturation arrest” early in neutrophil development in bone marrow – meaning their neutrophils don’t mature fully into fighting-capable cells that could combat infections as effectively as expected – this form typically responds well to G-CSF treatments.
IDIOPATHIC NEUTROPENIA
This form of neutropenia can appear at any point during one’s life for unknown reasons and affects both children and adults alike. Most patients respond well to G-CSF treatments; however long-term regimens may be required in some instances.
CYCLIC NEUTROPENIA
Cyclic neutropenia is another hereditary form of neutropenia that exhibits a cyclic pattern of fluctuating neutrophil counts with an average cycle length of 21 days, although variations among patients exist – some being neutropenic throughout and others having low neutrophil counts for only some days but normal blood counts overall.
The frequency of bacterial infections depends upon the length of a neutropenic period experienced; those experiencing longer neutropenic periods within their cycle suffer more frequently from infections than others.
Cyclic neutropenia occurs as a result of fluctuating rates of bone marrow stem cell production fluctuating at various frequencies; other blood cells like platelets or red cells may also demonstrate oscillatory behavior resembling a cyclical pattern.
While it may occur sporadically, in certain families it’s passed down with one parent having more than one child affected; just like with Kostmann syndrome patients with cyclic neutropenia can benefit from G-CSF treatment as an adjuvant therapy.
AUTOIMMUNE NEUTROPENIA
Autoimmune neutropenia refers to antibodies in the blood that directly attack neutrophils found within our own bodies. This form of neutropenia is particularly prevalent among infants under three months, yet typically does not result in serious bacterial infections.
Granulocyte-specific antibodies can be detected using different immunological blood tests performed in specialized laboratories. If these antibodies are identified, patients should remain under medical supervision but may not require antibiotics or G-CSF for treatment.
Depending upon the frequency and neutrophil counts, prophylactic antibiotic therapy may be prescribed by your treating physician. When severe infections arise, G-CSF treatment may also be indicated; typically blood counts return to normal within 2-3 years.
Autoimmune neutropenia can sometimes occur among young people (aged 20-40), typically women, and it often co-occurs with other disorders or conditions.
Symptoms of agranulocytosis
Agranulocytosis can cause symptoms of infection that can be sudden or gradual.
The symptoms could include:
- Chills and fever.
- A faster heart rate and faster breathing.
- Fatigue and muscle weakness.
- A sore throat (pharyngitis) as well as bleeding gums, and inflammation.
- Mouth ulcers and throat, which cause difficulty swallowing.
- A sudden drop in blood pressure (hypotension) is a condition that can cause you to feel lightheaded or weak, or even cause you to vomit.
Symptoms of neutropenia
Neutropenia does not cause any symptoms, but infections that can result from having it can. Infections that are repeated can be an indication of neutropenia.
It could be a sign of:
- Fever (febrile neutropenia).
- Fatigue.
- A sore throat (pharyngitis).
- Swollen lymph nodes.
- Anus ulcers or mouth cancers.
- The rash, swelling, and pain in the area of an infection.
- Diarrhea.
- Burning during urination or any other urinary signs (urgency or frequency).
- If you are suffering from mild neutropenia, you may contain enough neutrophils
What is the cause of agranulocytosis?
Agranulocytosis is a condition that occurs when your neutrophil count drops to levels that are dangerously low.
This may occur at any time:
The body doesn’t produce enough neutrophils to function effectively.
The neutrophils that you have are getting destroyed or die prematurely.
Agranulocytosis that is inherited:
Inheritable agranulocytosis is caused by issues with the gene your body requires to produce neutrophils. Agranulocytosis which is this type is congenital (present when you are born).
Infantile genetic agranulocytosis can be described as a rare form of inheritance the condition known as agranulocytosis. It’s also known as Kostmann syndrome, also known as congenital agranulocytosis. The newborns who suffer from this condition experience frequent infections with fevers, inflammation, and issues with their bones.
Acquired Agranulocytosis
Certain types of prescription medications trigger the condition known as agranulocytosis. Other health issues, infections as well as exposure to chemicals could result in severely low levels of neutrophils.
The causes of acquired agranulocytosis are:
- Autoimmune disorders, such as rheumatoid or lupus.
- Bone marrow diseases and bone marrow failure diseases such as anemia with aplastic.
- Bone marrow, including leukemia.
- Treatments for cancer with chemotherapy.
- Chemicals or toxins like mercury or lead.
- Infections like tuberculosis, malaria, as well as Rocky Mountain spotted fever.
- Vitamin deficiencies and poor nutrition include Vitamin B12 as well as folate.
- Prescription medications, such as antipsychotic drugs, antibiotics, and thyroid medication issues, as well as many others.
What is the cause of neutropenia?
Many factors can cause neutropenia, resulting in destruction, reduced production, or an abnormal accumulation of neutrophils.
Treatment for cancer and cancer treatment:
Chemotherapy for cancer is a typical reason for neutropenia. Alongside eliminating cancerous cells, chemotherapy may also cause the destruction of neutrophils and other healthy cells.
- Leukemia
- Chemotherapy
- Therapy with radiation
Drugs:
- Treatments for an overactive thyroid, like methimazole (Tapazole) as well as propylthiouracil
- Certain antibiotics, such as vancomycin (Vancocin) penicillin G, and the oxacillin
- Antiviral medications, like Ganciclovir (Cytovene) and the drug valganciclovir (Valcyte)
- Anti-inflammatory medications to treat conditions such as ulcerative colitis and rheumatoid joint and Sulfasalazine (Azulfidine)
- Certain antipsychotic medicines are available, including clozapine (Clozaril, Fazaclo, others) and chlorpromazine
- The drugs used to treat irregular heart rhythms, such as procainamide and quinidine.
- Levamisole, A veterinary drug that’s not allowed for human use for human use in the United States, but may be mixed with cocaine
Infections:
- Chickenpox
- Epstein-Barr
- Hepatitis A
- Hepatitis B
- Hepatitis C
- HIV/AIDS
- Measles
- Salmonella infection
- Sepsis (an excessive bloodstream infection)
Autoimmune illnesses:
- Granulomatosis and polyangiitis (formerly known as Wegener’s Granulomatosis)
- Lupus
- Rheumatoid arthritis
Bone marrow disorders:
- Aplastic anemia
- Myelodysplastic syndromes
- Myelofibrosis
Other reasons:
- The condition is present from birth like Kostmann’s Syndrome (a disorder that causes an insufficient production of neutrophils)
- Unknown causes, referred to as chronic neutropenia idiopathic.
- Vitamin deficiencies
- Spleen abnormalities
- Patients can suffer from neutropenia with a higher risk of getting sick. This is referred to as benign neutropenia.
What are the risk factors for agranulocytosis?
It is more prevalent in women, and in those whose mothers were as females at birth. All ages of people are susceptible to agranulocytosis.
Agranulocytosis tends to be more prevalent in those who:
Patients are receiving chemotherapy treatment to treat cancer.
Are suffering from autoimmune conditions (conditions that trigger an immune system that attacks parts of your body) like lupus or the rheumatoid joint?
Take certain prescription drugs, such as the antipsychotic clozapine (Clozaril(r)), the antibiotic trimethoprim/sulfamethoxazole (Bactrim(TM)), and the thyroid medication methimazole (Tapazole(r)).
What are the risk factors of neutropenia?
Neutropenia, also known as Agranulocytosis, is characterized by low levels of neutrophils – white blood cells responsible for fighting infections.
There are various risk factors that lead to neutropenia’s development such as:
- Medical Conditions: Certain medical conditions are associated with increased risks for neutropenia. This includes autoimmune diseases like Lupus and certain viral illnesses like HIV. Myelodysplastic Syndromes (MDS), Aplastic Anemia, and leukemia may all increase this risk as well.
- Treatment Options for Cancer: Chemotherapy and radiation therapies used to treat cancer may damage bone marrow, the site where blood cells are produced, resulting in neutropenia (low white blood cell count).
- Bone Marrow: Problems Bone marrow diseases like myelodysplastic and aplastic anemia may decrease neutrophil production and therefore reduce production overall.
- Medicines: Certain medicines that disrupt your immune system could contribute to neutropenia. Examples include antipsychotics, antibiotics, and anti-seizure drugs.
- Inherited Disorders: Genetic disorders may increase a person’s chances of neutropenia. Examples include cyclic neutropenia as well as extremely congenital neutropenia.
- Nutritional Deficiencies: Lacking folate, vitamin B12, or copper could hinder bone marrow’s ability to create neutrophils.
- Viral Infections: HIV and Hepatitis virus infections can both contribute to neutropenia by damaging bone marrow.
- Chemical Exposure: Experiments using chemicals or toxins may harm bone marrow and lead to decreased production of neutrophils.
- Radiation Exposure: Experimenting with radiation at high levels through injuries or medical treatments may result in bone marrow damage that leads to neutropenia.
- Certain Medical Treatments: Certain medical procedures, like bone, stem cell, or marrow transplantation, may temporarily induce neutropenia until their transplanted cells begin producing new
- Blood cells: Chronic kidney disease could alter neutrophil production, potentially resulting in neutropenia.
- Malnutrition: Malnutrition has the ability to disrupt blood cell development, particularly neutrophil production.
How can agranulocytosis be diagnosed?
The healthcare professional will perform the blood test, also known as an entire blood count (CBC), and a differential test to examine the number of neutrophils present in your blood. Agranulocytosis happens in cases where the total neutrophil count (ANC) is less than 100 neutrophils for every microliter of blood. Normally, patients are at least 1,500 neutrophils per microliter.
The doctor can also take a swathe from your bone marrow (bone marrow biopsy, aspirate) to determine if your bone marrow produces neutrophils. Bone marrow can be described as the tissue inside bones which is where blood cells are created. They’ll ask about your symptoms and medications, as well as recent illnesses and exposures to chemicals.
If your doctor believes that you are suffering from an inheritable type of disease, you might require genetic tests. This could involve either a skin biopsy or a blood test.
How can neutropenia be diagnosed?
The most commonly used test is a basic blood test, called a total blood count (CBC) with differential. Your doctor will conduct this test on a regular basis to assess your neutrophil count in the event that you have received chemotherapy.
Your doctor may recommend further tests if they’re not sure of the cause of your neutropenia. In this case, for instance, they might collect a sample from your bone marrow and study the cells with a microscope.
This test could aid your doctor in determining if neutrophils are forming differently in the bone marrow of your patient or are destroyed after being created. This test will help your doctor establish the diagnosis.
Table difference between neutropenia and agranulocytosis
| Characteristic | Neutropenia | Agranulocytosis |
|---|---|---|
| Definition | Low neutrophil count | Severe decrease in neutrophil count |
| Neutrophil Count | Below normal, but not extremely low | Very low, often less than 500 cells/mm³ |
| Severity | Can vary in severity | Always considered severe |
| Causes | Various, including chemotherapy, infections, bone marrow disorders | Often caused by drug reactions, autoimmune disorders, idiopathic cases |
| Symptoms | Increased infection risk, fatigue, fever | High fever, rapid heart rate, sore throat, malaise |
| Treatment | Address the underlying cause, growth factor medications | Immediate cessation of offending drug, antibiotics, treatment of the cause |
| Prognosis | Generally good with treatable causes | Depending on the cause, can be fatal without prompt treatment |
| Long-Term Impact | Recurrent episodes possible | This can lead to serious complications |
Treatment of agranulocytosis
If you suspect that a prescribed medication is making you feel uncomfortable it is essential to discontinue taking the medication. Consult your doctor on how to stop the medication in a safe manner.
Agranulocytosis treatment consists of:
- Antibiotics: If you suffer from an infection, your healthcare professional will prescribe antibiotics as well as other medicines to ease the symptoms.
- Granulocyte colony-stimulating factor (G-CSF): The doctor may suggest injecting an agent to aid in helping your body to produce more neutrophils. Your doctor might suggest filgrastim (Neupogen(r)) pegfilgrastim (Neulasta(r)) or lenograstim (Granocyte(r)).
- Immunosuppressants: When an auto-immune disorder triggers agranulocytosis your physician may recommend treatments that inhibit (calm) your immunity system like prednisone.
- Bone marrow transplants: If other treatments don’t work, you might require a bone marrow transplant. This procedure will receive bone the marrow of a donor so that your body is able to produce more neutrophils.
- Prevention of infection: Those suffering from aggranulocytosis need to be vigilant to stay clear of the spread of infection. Make sure to wash your hands regularly avoid crowds and cover your face when in public. Consult your physician about any additional steps you may use to stay away from becoming sick.
Treatment of neutropenia
Certain types of neutropenia may need treatment. The treatment options you have are based on the cause of the low levels of neutrophils.
Treatments could consist of:
- Antibiotics: Antibiotic therapy can save your life if you suffer from neutropenia that is accompanied by fever (febrile neutropenia). Your doctor may refer you to the hospital where you’ll receive antibiotics intravenously (through the vein) to treat your illness and be tested to determine if you have the possibility of infection.
- Corticosteroids: Your doctor may prescribe corticosteroids if your condition is an autoimmune disease. These medications can block (lessen) the body’s immune system which causes the destruction of neutrophils.
- Granulocyte colony-stimulating factors (G-CSF): A doctor might also prescribe medications that stimulate the production of cells called white blood cells within the bone marrow. It is likely that you will receive G-CSF if your treatment includes chemotherapy.
If your medication is causing neutropenia, your physician may suggest that you take it off, or adjust your dosage.
Final outline – Neutropenia vs. Agranulocytosis
White blood cells form a component of the immune system in the body. They help the body fight infections as well as other illnesses.
White blood cells found in the human body are the granulocytes (neutrophils and eosinophils), basophils monocytes, as well as lymphocytes (T cells and B cells).
Neutropenia and agranulocytosis are both medical conditions that result from low levels of specific white blood cell types. In neutropenia patients, there is an insufficient amount of a granulocyte known as neutrophils.
In the condition of agranulocytosis, there are very low levels of all granulocytes including basophils and neutrophils as well as Eosinophils. This is the difference between neutropenia and aggranulocytosis.