Thalassemia and Anemia: Red Blood Cells, also known as RBCs, serve an important function in our bodies, oxygen transport. RBCs bind oxygen molecules from our lungs and transport them throughout various tissues throughout our bodies – acting like transport tubes! Anemia occurs due to low RBC numbers; severe anemia can result in cardiac arrest when left untreated while Thalassemia causes extreme anemia as it cannot be effectively treated; using simple blood testing that measures hemoglobin can detect anemia quickly.
What Is Thalassemia?
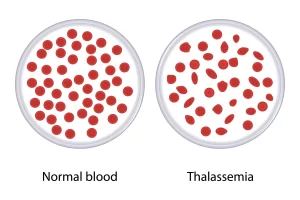
Thalassemia, a genetic blood condition, is distinguished by abnormal production of hemoglobin; hemoglobin serves to carry oxygen throughout your body’s cells. Thalassemia results from mutations to genes responsible for producing hemoglobin which causes reduced or absent production, eventually leading to symptoms like anemia.
Thalassemia comes in two varieties – alpha and beta.
Alpha Thalassemia occurs when alpha-globin chains, one of the key building blocks of hemoglobin, become deficient or missing altogether.
Alpha Thalassemia can be divided into various subcategories including:
Alpha
- Genes that affect carriers tend not to manifest any symptoms.
- Alpha-thalassemia involves two genes being affected and can result in mild anemia.
- Hemoglobin-H disease involves three genes and can range from mild to severe anemia.
- Alpha-thalassemia Major (also referred to as hydrops fetalis) affects all four genes and leads to severe anemia that is usually fatal during gestation or shortly thereafter.
Beta
- Beta Thalassemia, also known as Alpha Thalassemia, results from an insufficient or absence of beta-globin chains in the blood. There are two subtypes of Alpha Thalassemia;
- The gene mutation typically manifests itself with mild, nonsymptomatic anemia.
- Beta-Thalassemia Major (also referred to as Cooley anemia) is an anemia condition caused by both genes being affected, leading to serious anemia that requires regular transfusions as well as ongoing medical treatments.
- Thalassemia can be passed from parent to child through inheritance; depending on which genetic mutations were passed along by both, its severity varies widely; symptoms include fatigue, paleness, energy deficiencies and slow growth rates as well as jaundice or spleen enlargement.
- Blood tests can be used to diagnose thalassemia by measuring hemoglobin and looking for abnormal types. Additional diagnostic testing, including DNA analyses, may also be undertaken to detect genetic mutations.
Treatment options will depend on the severity and type of thalassemia; depending on its severity and type, potential therapies include blood transfusions for increasing hemoglobin, iron removal via frequent transfusions (chelation), or supplementing with folic acid. In rare instances bone marrow transplantation might even be an option; those living with the disorder or at risk should receive genetic counseling to address potential birth defects in future offspring.
What Is Anemia?
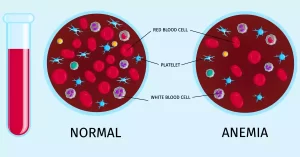
Anemia, a commonly found blood condition, can be defined as any decrease in red blood cell count or hemoglobin content – two components that provide oxygen transportation between lung tissue and tissues via red blood cells. Anemia may be the result of various factors and severity can range anywhere between mild and severe cases.
Anemia can manifest itself in various forms; most commonly:
- Anemia due to iron deficiency: When your body does not create enough hemoglobin owing to low iron levels, red blood cell numbers decline or become paler and smaller than they would typically be. This results in reduced production as well as paler red cells than desired.
- Anemia due to vitamin deficiency: Lacking folate or vitamin B12 can contribute to red blood cell formation problems and DNA production issues, ultimately leading to anemia. Both B12 and folate play an essential role in maintaining normal nerve cell functioning as well as producing DNA – depriving these essential vitamins can cause red blood cell production issues that hinder red blood cell formation and even cause some cases of neurological disorders such as dementia and nerve cell degeneration.
- Chronic Disease-Induced Anemia: Cancer, kidney disease, rheumatoid arthritis, and chronic inflammation can wreak havoc with our ability to make red blood cells or absorb iron, leading to anemia in its wake.
- Anemia Hemolytic: This form of anemia occurs when red blood cells die prematurely due to genetic mutation, autoimmunity disease, infection or medications or environmental toxins affecting them. It can result from inheritance disorders, autoimmune conditions or medication side-effects, infections, or pesticide exposures.
- Aplastic Anemia: This rare illness in which bone marrow fails to produce sufficient red, white, or platelet blood cells results in inadequate production of these blood types by your body. Anemia symptoms depend on their severity and cause; common anemia symptoms include fatigue, weakness, and pale skin.
Anemia can be identified through medical history review, physical exams, and blood tests that measure hemoglobin (the number of red blood cells), among other parameters. Additional diagnostic tools exist such as iron studies, vitamin level analyses, or bone marrow biopsies to detect its causes.
Anemia treatment depends on its severity and cause; such treatments could include iron and vitamin supplements, transfusions of blood, medications or alternative therapies to address its root causes; lifestyle modifications (dietary or chronic disease management); as well as regular follow-ups with healthcare professionals in order to properly manage anemia and monitor it.
Why does Thalassemia qualify as a disease?
Over centuries of study and management of thalassemias and anemias, advances have been made that have led to significant advances in the management of this rare blood condition. Here is a short introduction to thalassemia.
What is the History of Thalassemia?
- The term thalassemia was first coined during the early twentieth century when Thomas Cooley, Pearl Lee, and others coined this name after witnessing several patients suffering from severe anemia with large spleens.
- Thalassemia was originally studied as a hereditary illness by researchers in the 1950s. Researchers later realized it is caused by abnormalities in hemoglobin production which allows oxygen-carrying red blood cells to access oxygen more readily.
- Scientists eventually came to realize there are various forms of Thalassemia with genetic roots, with alpha and beta being two predominant varieties, each with subtypes and differing degrees of severity.
- Since the second half of the 20th century, genetic and prenatal tests have proven invaluable tools in early diagnosis and prevention – especially important in regions with higher incidence rates for thalassemia.
- Over time, thalassemia treatment has evolved greatly. Transfusions, iron chelation therapies, and bone marrow grafts have all become mainstream techniques to manage and enhance quality of life and manage thalassemia effectively.
What is the History of History of Anemia?
- Since ancient history began being recorded, anemia has been recognized and understood. Ancient medical texts like Ebers Papyrus of Ancient Egypt (1550 BCE) include references to anemia symptoms as early as 1550 BCE.
- Researchers began investigating different causes and types of anemia during the late 19th century. Anemia may result from blood loss, nutritional deficiency or problems inherent to blood cell production and destruction processes.
- Early 20th-century laboratory advances enabled hemoglobin measurement as an indispensable diagnostic tool in anemia cases.
- Over the course of the 20th Century, specific causes for different anemias were slowly unlocked. Iron deficiency anemia quickly emerged as one of the primary forms, due to inadequate iron absorption or intake.
- Medical science has advanced significantly in its understanding of anemia over time. Specific types are treated using nutritional supplements like B12 and iron to increase red blood cell production. Over time, management techniques that support red blood cell production have advanced considerably as have treatments to increase red cell counts.
- With ongoing medical advances and research, thalassemia, and anemia continue to evolve with treatment advances that aim to promote early diagnosis, effective prevention measures and quality-of-living improvements for those affected by these diseases.
What is the Difference between Thalassemia and Anemia?
Anemia and Thalassemia each present different challenges when it comes to blood disorders. Some key differences include:
Underlying Causes:
- Thalassemia is caused by genetic mutations involving hemoglobin-producing genes.
- Anemia can be caused by a variety of factors, including dietary deficiencies, chronic illnesses, autoimmune disorders, infections, drugs, or hereditary abnormalities.
Types and Subtypes:
- Thalassemia can be divided into two general types, Alpha and Beta. Within both types, many subtypes exist depending on which genetic mutations have been passed from parent to child.
- Anemia can be caused by a variety of factors, including iron shortage and vitamin deficiencies (e.g. B12 or folate deficiencies). Other forms include chronic disease-induced anemias as well as hemolytic anemia or even septic anemias.
Hemoglobin production and functionalities:
- Thalassemia (thalassemia): This abnormal condition results from improper or reduced production of alpha and beta chains of hemoglobin; thus producing inadequate or dysfunctional results in its subsequent form.
- Anemia: Low production or insufficient amounts of hemoglobin within red blood cells leads to reduced oxygen transport capabilities and ultimately anemia.
Affective severity and clinical manifestations:
- Thalassemia severity varies significantly according to subtype and mutation type; its symptoms also range in intensity based on these characteristics.
- Anemia severity varies based on its source, nutrition status, and general health factors. Anemia symptoms include weakness, weariness, pallor, dizziness, and a fast pulse.
Tests and Diagnostic Criteria:
- Blood tests used to diagnose thalassemia consist of measuring hemoglobin and testing abnormal hemoglobin. If necessary, genetic mutations can also be verified through DNA testing.
- Blood tests can be used to assess hemoglobin concentration and red blood cell counts as well as any relevant parameters, while additional diagnostic tools including iron studies, vitamin levels testing, and bone marrow biopsies may be employed in order to pinpoint its source.
Treatment and Management:
- Thalassemia treatment may include blood transfusions to increase hemoglobin, removal of iron through transfusions or supplementation with folic acids, and even bone marrow transplantation.
- Anemia treatment varies based on its severity and root causes, from supplementing iron or vitamin-deficient diets with supplements like iron and/or vitamins to managing chronic illnesses with medications tailored specifically for them, to administering other therapies designed to target its causes.
Thalassemia and anemia must be understood clearly to enable precise diagnosis and treatment, with individuals living with either being evaluated by healthcare professionals or receiving guidance as necessary.
Symptoms of Thalassemia
There are various types of thalassemia and their symptoms may differ widely; below are a few common ones associated with each subtype of this blood disorder.
Alpha Thalassemia:
- Silent Carrier (Asymptomatic): These cases do not manifest with symptoms or visible indicators.
- Alpha Thalassemia Trait (ATT): Characterised by mild anemia and fatigue; occasionally slight jaundice may develop (yellowing of skin or eyes).
- Hemoglobin-H Disease: Moderate to severe anemia with weakness and fatigue; pallid or yellow skin color, an enlarged spleen in serious cases (which could potentially block drainage of urine); bone deformities and jaundice.
- Alpha-thalassemia (hydrops fetal): is an anemia syndrome characterized by severe anemia, intrauterine growth restrictions, abnormal facial features and fluid buildup within the body resulting in liver, and spleen enlargement. Unfortunately, it often proves fatal shortly after birth.
Beta Thalassemia:
- Beta Thalassemia normally presents with mild symptoms, including fatigue and anemia.
- Beta Thalassemia (Cooley’s Anemia) is an anemia syndrome characterized by severe anemia and fatigue, along with weakness and pale skin. Other symptoms may also present.
- Important to know, some individuals with thalassemia might show no symptoms at all or only mild ones, even among people who share similar forms. Furthermore, symptoms and severity can differ considerably even within groups who share an identical form. Regular medical assessments and check-ups must take place for proper management and diagnosis of this form of blood cancer.
Symptoms of Anemia
Anemia symptoms depend on both its cause and severity as well as individual factors; anemia itself may manifest through various signs and symptoms that range in intensity from fatiguedness and shortness of breath to decreased memory or impaired concentration.
- Fatigue and Weakness: Even with sufficient rest and sleep, you may still feel exhausted or weak. Even simple daily activities may become tiring over time.
- Pale Skin: Pale skin refers to any condition whereby one’s skin becomes pale, such as lips, face, nails, gums or inner eyelids. It may affect lips, face, nails gums and eyelids – this could include lips, faces, nails gums gums as well as inner eyelids if present.
- Shortness of Breath: Breathlessness or difficulty catching one’s breath during physical activity or mild exercise are signs that there may be a difficulty.
- Rapid or Irregular Heartbeat: Anemia may contribute to irregular heartbeat patterns or increased speed, prompting it to beat quickly or irregularly.
- Lightheadedness or Dizziness: Feeling dizzy when standing up, especially after physical exertion has begun, is often caused by lightheadedness or dizziness. If this occurs for you when working, try lying down for at least ten minutes until the sensation passes.
- Headaches and Concentration Issues: Substantiated headaches, inability to focus, impaired memory function and decreased cognitive functionality are symptoms that must be managed regularly in order to function optimally.
- Cold hands and feet: Lower blood supply may contribute to feelings of coldness in hands and feet.
- Brittle Nails and Hair Loss: Individuals suffering from anemia often experience hair loss as part of the symptoms.
- Chest Pain: Angina or chest pain may result from inadequate oxygen delivery to the heart in severe anemia cases.
- Weakness or Exercise intolerance: Indicated by reduced muscle strength and endurance as well as difficulty performing physical activities, this issue results in inability to participate in physical activities or achieve them effectively.
These symptoms of anemia may differ depending on its cause; specific manifestations could also arise depending on its source. It’s advisable to seek professional medical advice if any of the listed signs occur for you.
When to see a doctor for Thalassemia?
If you believe that you or someone you know has Thalassemia, get medical attention right once to acquire an accurate diagnosis and treatment options.
- Families at Risk: Testing should be considered if there are known relatives with Thalassemia, or if you belong to ethnicities known for high rates of Thalassemia risk such as Mediterranean, Southeast Asian or Middle Eastern backgrounds.
- Unusual symptoms: If your kid or you have thalassemia symptoms such as weariness, pallor, weakness, poor growth rate, jaundice, or an enlarged liver, it is critical that you should get a medical attention right once.
- Abnormal Blood Test Results: Abnormal Blood Test Results If your results for blood tests reveal low hemoglobin or an unusual index of red blood cells, this could indicate the presence of thalassemia.
When to see a doctor for Anemia?
- Consistent symptoms: Anemia’s persistent symptoms such as fatigue or weakness, pallor, dizziness or rapid heartbeats, cold hands or feet and shortness of breath may continue or even worsen over time.
- Unexplained Causes: Even though you cannot pinpoint its exact origins, the symptoms could possibly be the result of chronic illness, nutritional deficiency or another factor.
- High-Risk Groups: If you have anemia-causing disorders such as chronic kidney disorder or an autoimmune disease or are taking certain drugs that increase anemia risks, you could fall under one of the high-risk groups for anemia.
- Iron and Vitamin Deficiencies: Are You Concerned about Iron Deficiencies and Vitamin Inadequacies, Which Can Lead to Anemia? This may be particularly true if your diet includes strict vegetarian or vegan food requirements, or if other special dietary needs exist within your community.
Healthcare professionals can only properly identify thalassemia and anemia with accuracy while offering suitable treatments. A thorough assessment process includes reviewing past medical histories, physical exams, and blood testing in order to ascertain the cause and severity of the disease. Early identification and management can improve quality of life and outcomes significantly.
What is the Treatment of Thalassemia?
Thalassemia treatment varies based on severity and type. Below are the mainstay treatments of thalassemia.
Blood Transfusions: For individuals suffering from moderate or severe thalassemia, regular blood transfusions are an integral component of treatment. Transfusions help improve oxygen-carrying capacity as well as red blood cell count by adding new red cells into circulation – these transfusions may take different frequencies or amounts depending on an individual’s situation.
Iron Chelation Therapy: Iron Chelation Therapy may help your body rid itself of excess iron through blood transfusions or frequent medical treatments containing transfusion-derived iron, leading to iron overload in the system. Orally or intravenously administered chelation medications may be given in order to remove iron excess from the body and provide benefits of healing as a side effect.
Folic Acid: Folic acid is essential in supporting red blood cell production; individuals living with Thalassemia may benefit from supplementing their intake to aid their red cell count production.
Bone Marrow Transplantation: Under certain conditions of Thalassemia, bone marrow transplantation is sometimes recommended in severe cases. The procedure replaces damaged marrow cells with donor ones that produce normal red blood cell production – the process being reserved only for people suffering severe forms or high-risk versions.
Supportive measures: Additional supportive measures may be added to a treatment plan to enhance quality of living and manage complications more effectively, including regular organ monitoring, iron overload management strategies, vaccination against infections such as influenza or measles as preventative measures, nutritional support services or specific support for symptoms associated with thalassemia.
Treatment options for thalassemia depend on its severity, individual patient characteristics and provider expertise; usually developed through collaboration among various experts such as hematologists and genetic counselors.
Individuals living with thalassemia must attend regular follow-up appointments in order to assess treatment effectiveness and identify complications, while new approaches and advancements in managing this disease could alter treatment approaches over time.
What is the Treatment of Anemia?
Treatment of anemia depends on its severity and root causes; here are common treatments available.
Iron-Deficiency Anemia:
- In order to replenish iron reserves in the body, oral tablet or liquid form iron supplements may be prescribed and taken according to their directions and as indicated.
- Red meat, Poultry and fish along with beans, lentils and leafy green will help to increase iron intake by consuming these rich foods.
Vitamin Deficiency Anemias:
- Anemia caused by vitamin deficiencies may require supplements or injections as treatment options.
- Consume more folate- and vitamin B12-rich food items (such as citrus fruits, leafy greens, legumes, meat, and dairy products ) or products ( including animal products like beef, poultry pork milk, etc ). This will support health.
Anemia of Chronic Disease:
- Treating any chronic diseases that contribute to anemia, like kidney disease, inflammation or infections can help ameliorate symptoms and alleviate anemia altogether. For example- kidney health issues; inflammation issues or even infectious infections should all be tackled to promote better anemia levels.
- In some cases, ESAs, which are synthetic versions of the hormone erythropoietin, may be administered to boost red blood cell formation and raise red blood cell counts.
Hemolytic anemia:
- Whatever its source may be, hemolysis can often be managed effectively using medications and treatments tailored specifically for its cause – these may include controlling immune system activity, eliminating triggers that lead to hemolysis or managing condition directly.
Aplastic Anemia:
- Stem cells from Blood or Marrow: When treating severe forms of anemia, donor stem cells or harvested ones harvested directly by the individual may be transplanted as stem cell replacement therapy.
- Immunosuppressive Treatment: Antibody-suppressing medication may help suppress your immune system, decreasing bone marrow destruction.
Healthcare professionals should establish the treatment for anemia after proper evaluation and diagnosis, taking into account various forms of anemia as well as individual factors and types. In order to effectively manage anemia, regular follow-ups, monitoring blood counts closely, and addressing any potential underlying issues should all be part of ongoing management strategies.
Causes of Thalassemia
Let’s examine each condition separately:
Thalassemia results from genetic mutations which disrupt hemoglobin production – the oxygen-carrying protein within red blood cells. Gene mutations determine both its severity and type. Alpha and beta thalassemias both have distinct genetic causes.
- Alpha Thalassemia: Alpha Thalassemia, also known as alpha thalassemia, results from mutations to genes which control production of alpha globin chains. In most cases this condition runs in families when both parents carry defective alpha globin genes.
- Beta Thalassemia: occurs when mutations develop in genes responsible for producing beta-globin chains. The severity of beta thalassemia depends on which genes both parents have passed on with regards to specific mutations inherited.
Thalassemia may be passed from parent to child via autosomal-recessive inheritance, meaning an individual needs at least two copies (one each from both parents) of a defective gene to be affected by it.
Causes of Anemia
There can be various reasons behind anemia, including:
Nutritional Deficiencies:
- Iron Deficit: Lack or inadequate absorption of iron may result in anemia, leading to decreased hemoglobin production.
- Vitamin Deficiencies: An insufficient supply of essential vitamins such as B12, folate or other must-haves can impede red blood cell production and have detrimental consequences on health.
Chronic conditions or diseases:
- Anemia from Chronic Inflammation: Chronic inflammation conditions like rheumatoid arthritis or Crohn’s can interfere with your body’s production of red blood cells and lead to anemia.
- Chronic Kidney Disease: Kidney dysfunction affects erythropoietin production, essential in creating red blood cells.
Bone marrow can become compromised due to cancer, HIV/AIDS or chronic diseases – leading to decreased red blood cell production and decreasing red blood cell counts in your system.
Hemolytic anemia:
- Inherited Disorders: An inherited disorder such as sickle-cell anemia or even (rarely) thalassemia and hereditary Spherocytosis may result in the early destruction of red blood cells causing hemolytic anemia while predisposing individuals to anemia itself.
- Autoimmune disorders: When our immune systems mistakenly attack red blood cells and destroy them, this is known as autoimmunity.
- Medications or Toxins: Some medications or toxins may contribute to red blood cell destruction.
Bone Marrow Disorders:
- Aplastic Anemia: Due to damage or suppression, bone marrow fails to produce enough red blood cells and therefore anemia occurs.
- Myelodysplastic Syndrome: Abnormal cell development and maturation within bone marrow causes red blood cell production to drop significantly, eventually leading to Myelodysplastic Syndrome and further reductions.
Here are the most frequently encountered causes of anemia, although other conditions and factors could also play a part. A healthcare professional will help identify its source through evaluation and testing services.
Risk Factors for Thalassemia
- Family History: Thalassemia can be passed from parent to child. A history of this disease in your family increases your likelihood, with children inheriting it if one or both parents carry mutations for it.
- Ethnicity: Certain ethnicities tend to have higher prevalences of Thalassemia; people of Mediterranean, Middle Eastern or Southeast Asian ancestry are at a greater risk.
- Consanguineous Marriage: Thalassemia Risk Increases When There Is Blood Relating Marriage, Thalassemia risks increase when there are consanguineous marriages between individuals who share genetic material; when both parents carry carriers of this gene it increases significantly the chances that one or both children could inherit it and develop it themselves.
Risk Factors for Anemia
Risk Factors of Anemia Anemia can often be traced back to nutritional deficiencies; factors that increase its risks include:
- Iron Deficiency Anemia, Iron deficiency may result from vegetarian or vegan diets; pregnancy, infants, and some digestive conditions that inhibit iron absorption.
- Vitamin Deficiency Anaemias (VDA) Malabsorption disorders and alcoholism play an integral part in VDA.
- Chronic illnesses or disorders that can induce anemia include- Anemia can be caused by chronic inflammatory disorders such as arthritis, Crohn’s disease, or ulcerative colitis.
- Anemia may be brought on by chronic infections like HIV/AIDS.
- Certain groups and genders tend to be more vulnerable than others to anemia.
- Anemia in infants and children may occur as the result of rapid development or inadequate nutrition.
- Iron deficiency in women of childbearing age can be an ongoing health problem. Pregnancy increases your risk for deficiency; menstruation also plays a part.
- Anemia affects older adults due to nutritional deficiencies, diseases, and medications they are taking.
- Anemia can result from significant blood loss due to menstruation, gastrointestinal bleeding, or surgery.
- Anemia can result from both genetic and acquired disorders, including sickle-cell disease, thalassemia, and hereditary Spherocytosis.
- Note that these risks are general estimates; individual risks will depend upon various factors and should always be discussed with health professionals for best practice advice. If you are worried about your own individual risk for thalassemia and anemia, make an appointment to talk with one today.
Conclusion
Anemia and Thalassemia can be distinguished as blood diseases that are characterized by a variety of reasons and signs. Anemia refers to a condition in which there is a lack of hemoglobin or red blood cells which is often caused by a variety of causes like iron deficiency. Thalassemia, however, on the contrary, on the other hand, is a genetic disorder that affects hemoglobin production. While both disorders result in decreased oxygen transport capacity in your blood vessels, Thalassemia is more specific to genetic mutations and anemia can result from different reasons. The correct diagnosis and treatment are vital to managing these conditions efficiently and enhancing the quality of life of patients affected.

